Artritis reumatoide
Produced by Rebecca Canvin, Bupa Health Information Team, January 2012.
This factsheet is for people who have rheumatoid arthritis, or who would like information about it.
Rheumatoid arthritis is a condition that affects joints and tissues around them. They become inflamed, which causes stiffness, pain and swelling.
About rheumatoid arthritis
Symptoms of rheumatoid arthritis
Causes of rheumatoid arthritis
Diagnosis of rheumatoid arthritis
Treatment of rheumatoid arthritis
Living with rheumatoid arthritis
Video
About rheumatoid arthritis
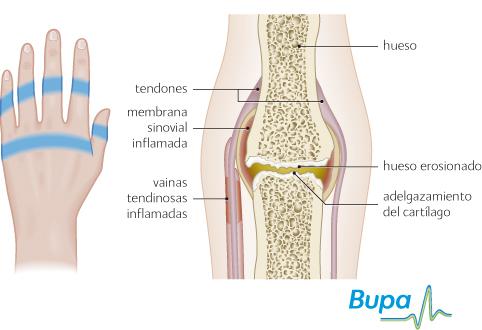
Rheumatoid arthritis is an inflammatory disease. It develops when your body's immune system starts to attack your joints and the tissues around them. Inflammation can affect the sacs of fluid (bursae) that help your muscles and tendons move easily over each other. It can also affect the lining of your joint (synovial membrane) and the tubes in which your tendons move (tendon sheaths).
When your joint and the tissue that surrounds it becomes inflamed, it turns red, swollen, warm to the touch and painful.
During this time, the capsule around your joint swells. When the swollen and inflamed tissue goes down the joint capsule remains enlarged. Inflammation can also affect other parts of your body as well as your joints.
Rheumatoid arthritis affects up to one in every 100 people, and is more common in developed countries. Rheumatoid arthritis is most likely to develop between the age of 30 and 50, although older and younger people can also develop the condition. It affects around three times as many women as men.
Symptoms of rheumatoid arthritis
Inflammation in rheumatoid arthritis may come and go. You may have periods where your condition flares up and your symptoms get worse. This may last several days or a few months. In between flare-ups the inflammation will go down and you will have fewer symptoms. This can last for months or years.
Rheumatoid arthritis is usually a symmetrical arthritis, which means it affects joints on both sides of your body at roughly the same time. Although it affects everyone differently, most people find that the joints in their hands and feet are affected. You may also have rheumatoid arthritis in your knees and shoulders, and less commonly in your hips, elbows and other joints. Most people have more than one joint with arthritis.
For many people, the condition develops quite slowly at first and you may notice only general symptoms like tiredness, aching joints and weakness. Other people find the condition comes on quickly and painfully, making it difficult to carry out daily activities. Common symptoms include:
- pain and swelling around the joint, making it tender and warm
- stiffness in the morning, or if you sit for a long time
- tiredness, making you feel irritable and depressed
- flu-like symptoms such as fever
Less common symptoms of rheumatoid arthritis include weight loss and rheumatoid nodules. These are fleshy lumps that usually appear on your hands, feet and elbows. Sometimes inflammation can develop in other areas of your body, such as your lungs and heart, but this is rare.
Causes of rheumatoid arthritis
The exact cause of rheumatoid arthritis isn't known. If you have rheumatoid arthritis in your family, you're more likely to develop the condition. However, certain lifestyle factors may also increase your risk of developing it. You may be more likely to develop rheumatoid arthritis if you smoke, eat a lot of red meat or drink a lot of coffee.
Some doctors believe that rheumatoid arthritis may be triggered by stress, an infection, a virus or hormone changes, but as yet there isn't any evidence to prove this.
Diagnosis of rheumatoid arthritis
If you think you may have rheumatoid arthritis, even if your symptoms are mild, see a doctor. It's important to be diagnosed as early as possible, as the sooner you start treatment the more effective it's likely to be.
Your doctor will ask about your symptoms and examine you. He or she may also ask you about your medical history. Rheumatoid arthritis can be difficult to diagnose and if your doctor thinks you may have the condition, he or she will refer you to see a rheumatologist, a doctor who specialises in treating the condition.
You may have a blood test. This is used to check whether you have anaemia or whether there is inflammation present in your body. A blood test can also be done to check whether you have a rheumatoid factor and anti-CCP antibodies. These are antibodies produced by a reaction in your immune system. Around eight out of 10 people with rheumatoid arthritis have one or both of these antibodies. You may also need to have an X-ray, ultrasound or MRI scan to look for changes in your joints.
Please note that availability and use of specific tests may vary from country to country.
Treatment of rheumatoid arthritis
There is no cure for rheumatoid arthritis. However, there are a number of treatments that can help to control your symptoms. Treatment can also slow down the development of the condition and minimise the damage to your joints. The earlier you start treatment the more effective it will be.
Self-help
There are many things you can do to reduce pain and stiffness in your joints, and to make day-to-day life easier. Self-help measures can help to reduce the stress on your joints and reduce the severity of your condition. Some of the main ones are listed below.
- Try to maintain a healthy weight for your height. This may mean losing weight if you're overweight. Extra weight puts more stress on your joints and can make rheumatoid arthritis worse.
- Find a balance between rest and exercise. Rest will help your joints feel more comfortable, but exercise can help to keep your joints working well. Swimming and aquarobics are good activities as they provide extra support for your joints. If you have pain when you're exercising or if a joint becomes warm and swollen, stop the exercise.
- Pace yourself. For example, spread out any chores that need doing, rather than trying to do them all at once.
- Eat a healthy, balanced diet. There is some evidence that omega-3 oils (for example fish oils) can help to ease joint pain and stiffness, though it can take a few months for you to see any benefit.
- Manage flare-ups. The longer you have rheumatoid arthritis the more likely it is that you will notice the early signs of a flare-up. This means you can take action quickly.
- Think about making changes to your car, home or workplace to ease any stress on your joints. You may be able to get help from an occupational therapist (a health professional who can give practical assistance to help you manage with everyday tasks and increase your independence).
- Use braces or supports for your joints to keep your joint stable and provide support. Ask a physical therapist (physiotherapist) about these.
- Manage tiredness. Rheumatoid arthritis can make you feel very tired and worn out, and you may find it difficult to do some day-to-day activities. Make sure you have a comfortable bed and a relaxing bedtime routine. Rest during the day when you need to.
- Use splints to support your joints when you're working or resting. These can relieve pain. Ask your doctor or physical therapist for more information about these.
Medicines
There are a number of medicines that can help to relieve your symptoms and some can prevent your condition from getting worse.
Painkillers, such as paracetamol (acetaminophen) and codeine, may help to ease your pain. Always read the patient information leaflet that comes with your medicine and if you have any questions, ask your pharmacist for advice.
Non-steroidal anti-inflammatory drugs
Non-steroidal anti-inflammatory drugs (NSAIDs) can also help to control your pain and stiffness. They work by reducing inflammation in your joints. However, they can't stop the arthritis from getting worse or affecting your joints. There are many NSAIDs available, including ibuprofen, naproxen and diclofenac. NSAIDs are usually prescribed at the lowest dose possible for short periods of time. This is because using them for long periods has been linked with heart, kidney and stomach problems. If you're taking NSAIDs regularly, your doctor may suggest taking a medicine called a proton pump inhibitor as well. This medicine protects your stomach and reduces the risk of side-effects from NSAIDs.
Disease-modifying anti-rheumatic drugs
There are other medicines available that can be used to slow down the development of rheumatoid arthritis and reduce your symptoms. Disease-modifying anti-rheumatic drugs (DMARDs) work by tackling the cause of inflammation in your joints. Most DMARDs work on your immune system, reducing the attack on your joints. Being treated early with DMARDs may help to reduce long-term damage to your joints, so it's important to start taking them as soon as possible after your diagnosis. They can take several weeks to have an effect, so keep taking them even if they don't seem to be working. You may need to take more than one of these medicines.
DMARDs include methotrexate, sulfasalazine, leflunomide, hydroxychloroquine sulphate, azathioprine and ciclosporin. If you're taking DMARDs, you should have regular blood and urine tests to check that your bone marrow, kidneys and liver are working well and to check for side-effects. When your condition is well controlled your consultant may reduce the dose of these medicines so that you're taking the smallest amount needed.
Biologic medicines
If DMARDs don't work well enough for you or you have side-effects from them, your doctor may suggest biologic medicines. These work by targeting certain chemicals that cause inflammation. You can take biologic medicines on their own, but they are often given with DMARDs. Biologic medicines are given by injection and include infliximab, etanercept, adalimumab, certolizumab, rituximab, golimumab and tocilizumab.
Corticosteroids
Your doctor may also suggest corticosteroids, particularly during a flare-up. These work by reducing inflammation. You can take them as tablets or they can be given as an injection into a painful joint. This can help to reduce pain and inflammation while you are waiting for other treatments to start working. Corticosteroids can have side-effects when used for long periods of time, so your doctor will give you the lowest effective dose and monitor you closely. Don't stop taking corticosteroids suddenly.
Surgery
You may be offered surgery as part of your treatment, usually if other treatments haven't worked. Operations vary from minor procedures to remove the inflamed lining of a joint, to more major surgery to replace a joint. Talk to your doctor for more information.
Physical therapies
A physical therapist can give you exercises that will help you to stay flexible and build up your muscle strength. He or she can also help you to improve your general level of fitness.
A podiatrist, a health professional who specialises in conditions that affect the feet, can help with any problems with your feet. This includes advice about shoes and help to find the right footwear for you.
Complementary therapies
Many people with rheumatoid arthritis use complementary medicines to ease their symptoms. Complementary therapies such as acupuncture, aromatherapy and massage may relieve pain and stiffness and make you feel more relaxed. However, they have no effect on how your condition develops. Speak to your doctor before trying any complementary therapy, as it may affect other medicines.
Availability and use of different treatments may vary from country to country. Ask your doctor for advice on your treatment options.
Living with rheumatoid arthritis
You may find day-to-day life with rheumatoid arthritis upsetting and frustrating at times. It can be an unpredictable condition because it comes and goes and you may not be able to plan ahead. Living with pain, discomfort and disability can affect you emotionally as well as physically and you may find that you become depressed. Talk to your doctor about how you're feeling and the impact that the condition has on your life.
You may find it helpful to contact support groups and organisations for information. Some of these organisations will be able to put you in touch with other people with rheumatoid arthritis. There are also self-management courses available for people with arthritis. These can help you to develop coping skills and manage your symptoms. Ask your doctor for more information.
An occupational therapist may be able to help you adapt your home and workplace to ease your symptoms and the stress on your joints.
Video
See our videos about rheumatoid arthritis, they include:
Should I exercise if I have arthritis?
What exercises can I do for arthritis in my hands, wrists and forearms?
What exercises can I do for arthritis in my shoulders?
What exercises can I do for arthritis in my back?
What exercises can I do for arthritis in my knees?
Publicado por el equipo de Bupa de información sobre la salud, noviembre de 2009.
Esta sección contiene respuestas a preguntas frecuentes sobre este tema. Las preguntas fueron sugeridas por profesionales de la salud, comentarios en el sitio web y consultas por correo electrónico.
Si tengo artritis reumatoide (AR), ¿debo ver a un terapeuta ocupacional?
Respuesta
Sí, un terapeuta ocupacional puede ser muy útil, especialmente si usted tiene problemas con las actividades cotidianas.
Explicación
Los terapeutas ocupacionales son profesionales de la salud que puede ofrecer asistencia práctica para ayudarle a manejar sus tareas diarias y aumentar su independencia. Según la Ley de SNS y Asistencia Social de 1990, usted tiene derecho a una evaluación de necesidades de servicios sociales.
Un terapeuta ocupacional evaluará su enfermedad antes de analizar sus necesidades en su hogar o de transporte, aficiones y trabajo. Luego le ofrecerá consejos prácticos para:
- adoptar una nueva postura durante la realización de actividades como cocinar
- descansar lo suficiente
- proteger sus articulaciones
- utilizar dispositivos y adaptaciones en el trabajo y el hogar (incluyendo las adaptaciones para los automóviles): los Centros locales de vida para discapacitados ofrecen la oportunidad de probar dispositivos y también se puede obtener asesoramiento en los Centros de Movilidad
- férulas para aliviar la tensión y el dolor en las articulaciones de la mano y muñeca mientras lleva a cabo las actividades y para mantener sus articulaciones estables cuando descansa
Información adicional
Arthritis Care
0808 800 4050
www.arthritiscare.org.uk
Arthritis Research Campaign (Campaña para la Investigación de la Artritis)
0870 850 5000
www.arc.org.uk
Disabled Living Centres (Centros de vida para discapacitados)
0870 770 2866
www.assist-uk.org
The Forum of Mobility Centres (Foro de Centros de Movilidad)
0800 559 3636
www.mobility-centres.org.uk
Ricability
020 7427 2460
www.ricability.org.uk
Fuentes
Occupational therapy and arthritis. Arthritis Research Campaign. www.arc.org.uk, consultado el 7 de julio de 2009
Occupational therapy. Arthritis Care. www.arthritiscare.org.uk, consultado el 7 de julio de 2009
In the home. Arthritis Care. www.arthritiscare.org.uk, consultado el 7 de julio de 2009
¿La artritis reumatoide (AR) afectará todo mi cuerpo?
Respuesta
Es difícil de decir, ya que la AR afecta a todos de manera diferente.
Explicación
Una vez que avanza, la AR puede extenderse a otras articulaciones. Sin embargo, existen muchos tratamientos eficaces que pueden reducir su efecto.
En muy raras ocasiones, la inflamación puede afectar sus ojos, secándolos e irritándolos, y sus glándulas lacrimales, glándulas salivales, vasos sanguíneos, pulmones e incluso el corazón.
La mayoría de las personas con AR tienen otros problemas generales, tales como rigidez, cansancio y malestar. Sin embargo, los medicamentos le ayudarán a controlar la AR. Su fisioterapeuta y terapeuta ocupacional también pueden darle consejos sobre cómo hacer cambios en su estilo de vida para aliviar los síntomas.
Información adicional
Arthritis Care
0808 800 4050
www.arthritiscare.org.uk
Arthritis Research Campaign (Campaña para la Investigación de la Artritis)
0870 850 5000
www.arc.org.uk
Fuentes
Rheumatoid arthritis. Arthritis Research Campaign. www.arc.org.uk, consultado el 7 de julio de 2009
Rheumatoid arthritis. Arthritis Care. www.arthritiscare.org.uk, consultado el 7 de julio de 2009
¿El ejercicio empeorará mi artritis reumatoide (AR)?
Respuesta
No, siempre que lo haga con cuidado. Está comprobado que el ejercicio es beneficioso si tiene artritis reumatoide. La clave está en encontrar un equilibrio entre el ejercicio y el descanso.
Explicación
Las articulaciones inflamadas se benefician del reposo, pero si no las mantiene en movimiento, se pondrán rígidas y sus músculos se debilitarán.
Obtenga asesoramiento diseñado específicamente para usted: un fisioterapeuta puede ayudarle con esto. No obstante, no realice deportes de contacto y vigorosos, como fútbol y squash. La natación es, sin duda, la mejor forma de ejercicio ya que el agua soporta su peso.
Un programa de ejercicios debería incluir lo siguiente.
- Ejercicios de fortalecimiento para trabajar los músculos que rodean las articulaciones afectadas y mejorar la estabilidad y la movilidad, reduciendo el dolor y la discapacidad.
- Ejercicios de amplitud de movimiento para mantenerse flexible y en movimiento: hacerlos en la mañana puede ayudar a aliviar la rigidez y antes de irse a la cama puede ayudar a prevenirla.
- Ejercicio aeróbico que aumente su ritmo cardíaco y le deje levemente sin aliento: esto ayuda a reducir el dolor y mejorar su salud. Caminar, hacer yoga y montar en bicicleta o realizar las actividades cotidianas como las tareas domésticas o la jardinería pueden ayudar.
Estos son algunos consejos que podrían ayudarle cuando hace ejercicio.
- Integrar el ejercicio a su rutina diaria e ir aumentando lentamente.
- Tomar un baño o una ducha caliente, o colocar una botella de agua caliente sobre las articulaciones afectadas antes de hacer ejercicio.
- Nunca forzar una articulación dolorosa. Es normal sentir algo de dolor a medida que aumenta su programa de ejercicios. Sin embargo, si el dolor dura más de dos horas luego de hacer ejercicios, consulte a su médico de cabecera.
- Utilice siempre zapatos acolchados y que sujeten bien el pie.
Información adicional
Arthritis Care
0808 800 4050
www.arthritiscare.org.uk
Arthritis Research Campaign (Campaña para la Investigación de la Artritis)
0870 850 5000
www.arc.org.uk
Fuentes
Rheumatoid arthritis. Arthritis Research Campaign. www.arc.org.uk, consultado el 7 de julio de 2009
Keeping active. Arthritis Care. www.arthritiscare.org.uk, consultado el 7 de julio de 2009
Exercise and arthritis. Arthritis Care.www.arthritiscare.org.uk, consultado el 7 de julio de 2009
Temas relacionados
Artritis reumatoide
Osteoartritis
Artritis psoriásica
Esta información fue publicada por el equipo de Bupa de información sobre la salud, y está basada en fuentes acreditadas de evidencia médica. Ha sido sometida a revisión por pares, por parte de médicos de Bupa. Este contenido se presenta únicamente con fines de información general, y no reemplaza la necesidad de consulta personal con un profesional de la salud calificado.
Fecha de publicación: Noviembre de 2009.
Hoja informativa sobre la artritis reumatoide
Related topics
Anaemia – a general overview
NSAIDs
Osteoarthritis
Psoriatic arthritis
Further information
Arthritis Care
0808 800 4050
www.arthritiscare.org.uk
Arthritis Research Campaign
0870 850 5000
www.arc.org.uk
Sources
- Chronic rheumatic conditions. World Health Organization, accessed 30 July 2012
- Rheumatoid arthritis. Arthritis Research UK. www.arthritisresearchuk.org, accessed 10 August 2011
- Rheumatoid arthritis. Arthritis Care. www.arthritiscare.org.uk, published February 2011
- Living with rheumatoid arthritis. Arthritis Care. www.arthritiscare.org.uk, published April 2010
- Rheumatoid arthritis. eMedicine. www.emedicine.medscape.com, published August 2011
- Rheumatoid arthritis. Prodigy. www.prodigy.clarity.co.uk, published June 2009
- Management of early rheumatoid arthritis. Scottish Intercollegiate Guidelines Network (SIGN), February 2011. www.sign.ac.uk
- The management of rheumatoid arthritis in adults. National Institute for Health and Clinical Excellence (NICE), February 2009. www.nice.org.uk
- Looking after your joints. Arthritis Research UK. www.arthritisresearchuk.org, accessed 10 August 2011
- Taking care of joints. Arthritis Care. www.arthritiscare.org.uk, published January 2011
- Simon C, Everitt H, Kendrick T. Oxford handbook of general practice. 2nd ed. Oxford: Oxford University Press, 2007: 572
- Keeping active. Arthritis Care. www.arthritiscare.org.uk, published April 2011
















