Age-related macular degeneration (AMD)
This factsheet is for people who have age-related macular degeneration or who would like information about it.
Age-related macular degeneration (AMD) is a disease that affects a person’s ability to see what is directly in front of them – their central vision. It’s the most common cause of blindness in people over 60 in the Western world.
About age-related macular degeneration
Symptoms of age-related macular degeneration
Complications of age-related macular degeneration
Causes of age-related macular degeneration
Diagnosis of age-related macular degeneration
Treatment of age-related macular degeneration
Prevention of age-related macular degeneration
About age-related macular degeneration
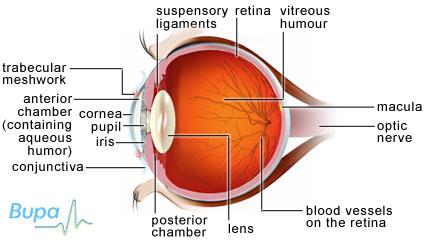
When light travels through your pupil it’s focused onto your retina, which is located at the back of your eye. The retina sends signals to your brain that are interpreted as vision. The macula is a small (about 0.5cm wide) spot in the centre of the retina that processes sharp, clear vision. When you look directly at something, the light is focused on the macula, allowing you to see fine detail and colour.
With AMD, the macula cells become damaged, leading to gradual loss of your central vision.
AMD affects about 20 to 25 million people worldwide. In the UK, around 500,000 people are thought to be affected by AMD. Around two in 100 people aged over 65 in the UK are blind in one or both eyes because of AMD.
Types of AMD
There are two main types of AMD:
Dry AMD is the most common type. It affects around nine out of 10 people with AMD. Your eyesight gradually worsens, becoming more blurred, over the course of five to 10 years. However, you may experience a slower deterioration in your sight.
Wet AMD happens when new blood vessels start to grow behind your retina. These can leak and cause scarring, damaging the macula. It may cause rapid and severe loss of your central vision.
Symptoms of age-related macular degeneration
AMD often affects both your eyes although it may affect one eye before the other. You may not notice at first as the good eye can mask the deterioration in your other eye.
Your symptoms may happen slowly over several months, but sometimes they develop more quickly. They include:
- distorted vision – straight lines become wavy or objects appear to be the wrong size
- blurry central vision
- seeing shapes or colours that aren't there
- seeing a dark patch or shadow when you wake which then fades
- difficulty reading, recognising people's faces, driving, looking at small objects and watching television
If you have any of these symptoms, see your GP or optician. AMD isn’t a painful condition. It also doesn’t usually lead to complete blindness because you still have your peripheral vision. This is what you can see to the sides.
Complications of age-related macular degener ation
AMD can lead to blindness if it’s left untreated. This is why it’s very important to visit your GP or optician if you have any symptoms.
Causes of age-re lated macular degene ration
No one knows exactly what causes AMD although it’s more common as you get older. However, there are a number of factors that can make AMD more likely. These include:
- smoking
- family history
- poor diet
- high blood pressure
- being of white ethnic origin
Diagnosi s of age-related macular degenerat ion
Your doctor will ask about your symptoms and examine you. He or she may also ask you about your medical history.
AMD may be detected during routine eye tests by your optometrist. He or she will check your level of vision and examine your macula using instruments to look inside your eye, sometimes using eye drops.
If AMD is suspected, you will be referred to an ophthalmologist (a doctor who specialises in identifying and treating eye conditions).
You may have other tests listed below.
- Amsler grid. This is a printed grid with a dot in the middle of it. You will be asked to describe any distortion, blank patches or blotches you can see on the grid when you look at the dot with one eye at a time.
- Fluorescein angiography. A dye called fluorescein is injected into your arm. This travels through your bloodstream to your eyes making the blood vessels inside your eye visible on a photograph so your ophthalmologist can identify the type of AMD.
- Ocular coherence tomography (OCT). This is a scan that shows your ophthalmologist detailed information about your macula.
Treatment o f age-related macular degene ration
Dry AMD
Currently there is no cure for dry AMD.
Your treatment will focus on helping you live with AMD and preventing it from getting worse.
Self-help
There are a number of things you can try that may help with your AMD. If you carry out close, detailed work you can use visual aids, such as advanced magnifying glasses and reading lights to make the best use of your vision. You may also find software that reads out text or displays large text helpful.
An occupational therapist can help to make every day living easier around your home.
Some research has found that vitamins A, C and E and beta-carotene and the mineral zinc and omega-3 fatty acids help to slow down the progression of AMD. Ask your ophthalmologist for advice about the correct dose and their side effects.
Wet AMD
Medicines
Your ophthalmologist can inject anti-VEGF medicines into your eye which can help to prevent wet AMD from progressing and even restore some lost vision.
Anti-VEGF medicines work by stopping new blood vessels growing and include:
- ranibizumab – now available on the NHS
- bevacizumab – being assessed in clinical trials
However, these medicines are only thought to be effective if they’re used during the early stages of the disease and may need to be injected every month to begin with.
Always ask your ophthalmologist for advice and read the patient information leaflet that comes with your medicine.
Photodynamic therapy (PDT)
PDT doesn't restore vision, but it can help stop wet AMD from getting worse. Your ophthalmologist will inject a special light-sensitive dye into your arm, which then travels to your retina. He or she will then focus a low-power laser on the macular area of the retina, destroying the abnormal blood vessels, without affecting the surrounding tissue.
You may need to have this treatment every three months if the blood vessels behind your retina continue to bleed.
Other treatments
Laser treatment is rarely used and only in the early stages of AMD to limit its progress. Heat from the laser destroys the blood vessels causing the AMD.
Researchers are looking into the benefits of stem cell therapy, combined therapy, gene therapy and surgical treatments for AMD.
Your ophthalmologist will be able to provide more information on which treatment is right for you.
Prevention of age-related macular degeneration
You can help reduce your chances of developing AMD by:
- stopping smoking
- eating plenty of brightly coloured fruit and vegetables, especially leafy green vegetables, eggs, and at least two portions of oily fish a week
- avoiding a high-fat, high-cholesterol diet
- asking your doctor or ophthalmologist about the correct dose of vitamin and zinc supplements
- wearing sunglasses in bright sunlight
- having an eye examination every two years so that its early signs can be picked up
Published by Bupa’s Health Information Team, September 2010.
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email. This section will expand over time.
How close are we to a cure for dry AMD?
My doctor told me I have dry AMD, will I go blind?
How will I cope with AMD?
How close are we to a cure for dry AMD?
Some experts estimate that a treatment may be available for the condition within the next ten years.
Explanation
Scientists are investigating treatments for AMD all the time. Some researchers are looking into why some early dry AMD develops into wet AMD. Some are focusing on gene therapy.
A major project in London is researching into stem cell therapy and hopes to have a treatment available in the next two years.
However, all of these treatments need to be clinically trialled to see how effective and safe they are before being made widely available.
Further information
-
The Macular Disease Society
0845 241 2041
www.maculardisease.org
Sources
- MD Support. What is macular degeneration? www.mdsupport.org, accessed 2 June 2010
- AMD.org – Macular Degeneration Partnership. www.amd.org, accessed 2 June 2010
- The London Project to Cure Blindness. www.thelondonproject.org, accessed 2 June 2010
My doctor told me I have dry AMD, will I go blind?
Although no one can predict exactly how the disease is going to progress, it’s rare to lose all of your vision because of dry AMD.
Explanation
Because AMD affects your macula, which is responsible for your central vision, you will usually retain some peripheral vision – what you can see at the sides. Dry AMD progresses slowly over the course of five to 10 years or more and may not affect your vision as severely as wet AMD.
Further information
-
The Macular Disease Society
0845 241 2041
www.maculardisease.org -
RNIB
0303 123 9999
www.rnib.org.uk
Sources
- Age related macular degeneration. BMJ Clinical Evidence. www.clinicalevidence.bmj.com, accessed 2 June 2010
- Age related macular degeneration. RNIB. www.rnib.org.uk, accessed 2 June 2010
How will I cope with AMD?
Getting in touch with patient groups can be a valuable source of help and support. Some of these are listed under Further information.
Explanation
Talking to other people in your position can help you learn to cope. Given time you will adapt to using your peripheral vision – what you see at the sides – and learn to make use of visual aids such as magnifying devices. Talk to your GP, ophthalmologist, occupational therapist or social worker for more advice about how to cope with daily living.
Further information
-
The Macular Disease Society
0845 241 2041
www.maculardisease.org -
RNIB
0303 123 9999
www.rnib.org.uk
Sources
- Living with AMD. AMD Alliance. www.amdalliance.org, accessed 2 June 2010
Age-related macular degeneration (AMD) factsheet
Visit the Age-related macular degeneration (AMD) factsheet for more information.
Further information
-
The Macular Disease Society
0845 241 2041
www.maculardisease.org
-
RNIB
0303 123 9999
www.rnib.org.uk
Sources
- Simon C, Everitt H, van Dorp F. Oxford handbook of general practice. 3rd ed. Oxford: Oxford University Press, 2010:972, accessed 2 June 2010
- Age related macular degeneration. www.maculardisease.org, accessed 2 June 2010
- Age related macular degeneration. Amresh Chopdar. BMJ 2003; 326:485–488. doi: 10.1136/bmj.326.7387.485. www.ncbi.nlm.nih.gov, accessed 2 June 2010
- Age related macular degeneration. BMJ Clinical Evidence. http://clinicalevidence.bmj.com, accessed 2 June 2010
- Age related macular degeneration. RNIB. www.rnib.org.uk, accessed 2 June 2010
- Age related macular degeneration. CKS. www.cks.nhs.uk, accessed 2 June 2010
- Age-Related Macular Degeneration: Guidelines for Management. February 2009. The Royal College of Ophthalmologists. www.rcophth.ac.uk, accessed 2 June 2010
- Age related macular degeneration. RNIB. www.rnib.org.uk, accessed 2 June 201
- Talks J, Koshy Z, Chatzinikolas K. Use of optical coherence tomography, fluorescein angiography and indocyanine green angiography in a screening clinic for wet age-related macular degeneration. Br J Ophthalmol 2007; 91:600–601. doi:10.1136/bjo.2006.108043
- TA155 Macular degeneration (age-related) – ranibizumab and pegaptanib: quick reference guide. www.nice.org.uk, accessed 2 June 2010
- Department of Health asks NICE to look into Avastin use for eye conditions. www.nice.org.uk, accessed 2 June 2010
- The London Project to Cure Blindness. www.thelondonproject.org, accessed 2 June 2010
- Living with AMD. AMD Alliance. www.amdalliance.org, accessed 2 June 2010