Anal cancer

Anal cancer is a rare form of cancer. Less than 800 people are diagnosed each year in the UK, although this number has been rising[1]. Anal cancer is more common in women, men who have receptive anal intercourse and in people whose immune system has been suppressed.[2] Anal cancer is closely linked with the human papilloma virus (HPV).
What is anal cancer?
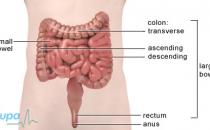
The anus is the name for the area at the very end of your bowel. The anal canal is the tube that connects the lower part of the large bowel (the rectum) to the outside of the body. It’s surrounded by a muscle called the sphincter which opens and closes to control your bowel movements.
Anal cancer is caused by the abnormal and uncontrolled growth of cells in the anus. The anal canal is lined with small, flat cells called squamous cells. Most anal cancers develop from these cells and are known as squamous cell carcinomas.
Where the anal canal meets the rectum is known as the transitional zone. Here, there are squamous cells and also glandular cells, which produce mucus to help your faeces pass smoothly through your anus. A type of cancer called adenocarcinoma of the anus can develop from glandular cells, but this is very rare. Two types of skin cancer called basal cell carcinomas or malignant melanomas can also occur around the anus, but these are also extremely rare (see Related topics).[3]
Symptoms
Anal cancers can cause you to have:[4] [5] [6]
- bleeding from your rectum, which you may see either on your faeces or on the toilet paper – this is the most common symptom of anal cancer
- pain in your anal area – a common symptom of anal cancer
- small lumps around your anus, which may be confused with piles (see Related topics)
- discharge of mucus or a jelly-like substance from your anus
- difficulty controlling your bowel movements (known as faecal incontinence)
- itchiness around your anal area
Although not necessarily the result of anal cancer, if you have any of these symptoms you should visit your GP.
Causes
The precise cause of anal cancer isn’t fully understood at present, but there are factors that may increase your chance of getting the disease.[7] [8]
- Human papilloma virus (HPV) –the virus that causes genital warts and is passed on from person to person through sexual contact. Over eight in every 10 people who are diagnosed with anal cancer have HPV infection in the anal area.[9]
- Number of sexual partners – the greater the number of sexual partners you have, the more likely you are to have an HPV infection.
- Anal intercourse – women who have anal intercourse and men who have receptive anal intercourse are at increased risk of developing anal cancer.
- Cancer of the vagina, cervix or penis – if you have a history of cervical or vaginal cancer or a history of penile cancer, you may be at increased risk of developing bowel cancer. This is because HPV is also associated with these cancers.
- Smoking – this increases your risk of getting anal cancer.
- Age – your risk of developing anal cancer increases with age.
- Immune system suppression – if you are taking medicines to suppress your immune system (eg after an organ transplant) or if you have HIV infection, you are at increased risk of getting anal cancer
Diagnosis
Your GP will ask about your symptoms and may examine you. He or she may also ask about your medical history. Your GP may refer you to a gastroenterologist – a doctor specialising in treating conditions of the bowel. You may need to have one or more of the following tests:[10] [11]
- An examination of your anus – rectal examination - your doctor will examine your anus with a lubricated gloved finger.
- A biopsy - the doctor will take a small sample of tissue from your anal area. This will be sent to a laboratory for testing.
- A CT (computerised tomography) scan - this uses X-rays to build up a three-dimensional picture of the anus.
- An MRI (magnetic imaging resonance) scan - this uses magnets and radiowaves to produce two and three-dimensional pictures of the inside of your body.
- An ultrasound – this uses sound waves to produce and image either of your abdomen, or you may have an endoanal ultrasound where a small probe will be passed into your anus for the scan.
Treatment
Non-surgical treatments[12]
The most common form of treatment for anal cancer is a combination of both chemotherapy and radiotherapy to kill the cancer cells. This is known as chemoradiation. They may be given to you at the same time or following one another. Chemotherapy uses anti-cancer drugs (known as cytotoxic drugs) which can be given by injection into one of your veins, or as tablets. Radiotherapy uses high energy rays to kill the cancer cells.[13]
Both treatments have side effects, however having both treatments together can sometimes make these side effects more severe. They may include:[14] [15]
- changes in your bowel habits, such as diarrhoea
- blistering and soreness of the skin around your anus
- tiredness
- loss of appetite
- feeling sick
- sore mouth and small mouth ulcers
- thinning or loss of hair
- narrowing and dryness of your vagina
Surgery [16] [17]
Chemoradiation is usually the preferred method of treating anal cancer. However, sometimes surgery may be needed to remove the cancer. There are two types of surgery. The operation you have depends on the size and position of your cancer.
An operation called a local resection is used to remove a small tumour and some of the surrounding tissue. This can only be done when your anal sphincter hasn’t been affected by the cancer. This type of surgery usually doesn’t affect your ability to pass a bowel movement.
Alternatively, the anus, rectum and part of the bowel can be removed by surgery. This is called an abdominoperineal resection. Without your rectum and anus you can’t pass a bowel movement and so the end of your bowel will be brought out onto the skin on the surface of your abdomen (tummy). This is called a colostomy and the opening of the bowel is known as a stoma. A bag is worn over the stoma and this collects your faeces. People with colostomies are able to live normal lives, including participating in sporting activities. [18] [19]
Prevention
There are several things you can do to reduce your risk of developing anal cancer.
You can:
- use a condom for sexual intercourse
- limit the number of sexual partners you have
- refrain from having anal intercourse
Stopping smoking will reduce your risk of getting anal cancer.
The information on the video provided does not constitute advice on diagnosis or the treatment for heart disease and such advice should always be sought from a doctor or another suitably qualified health professional.
Further information
-
Cancer Backup
0808 800 1234
www.cancerbackup.org.uk
Sources
-
Bowel Cancer UK
www.bowelcanceruk.org.uk
accessed 10 July 2007
-
Cancer Backup
www.cancerbackup.org.uk
accessed 20 Aug 2007 -
Cancer Research UK
www.cancerhelp.org.uk
accessed 20 Aug 2007 -
The American Cancer Society
www.cancer.org
accessed 22 Aug 2007 - Cassidy J, Bissett D, Spence R. Oxford Handbook of Oncology. 1st edition. Oxford: Oxford University Press, 2002
- Johnson L et al. Anal cancer incidence and survival: the surveillance, epidemiology, and end results experience, 1973-2000. Cancer. 101; 2:281-288. 2004
- Urions H, Bendell J. Anal Cancer: An Overview. The Oncologist 12:524-534. 2007
Related links
- Bowel Cancer
- Cancer – a general overview
- Chemotherapy
- CT scan HIV and AIDS
- MRI scan
- Radiotherapy
- Skin cancer
- Stoma care
- Ultrasound
http://www.cancerbackup.org.uk/Cancertype/Bowelcolonrectum, accessed 10 July 2007
http://www.bowelcanceruk.org.uk/patientpathways.htm, accessed 10 July 2007
This information was published by BUPA’s health information team and is based on reputable sources of medical evidence. It has been peer reviewed by [(insert reviewer(s) and patient groups if they have agreed), and by] BUPA doctors. The content is intended for general information only and does not replace the need for personal advice from a qualified health professional.