Back pain
This factsheet is for people who have back pain, or who would like information about it.
Back pain usually affects the lower back. It can be a short-term problem, lasting a few days or weeks, or continue for many months or even years. Most people will have some form of back pain at some stage in their lives.
About back pain
Symptoms of back pain
Causes of back pain
Diagnosis of back pain
Treatment of back pain
Prevention of back pain
About back pain
Back pain is extremely common – about four in five people are affected at some point in their lifetime. Anyone can get back pain at any age, but it’s most common in people between the ages of 35 and 55, or over.
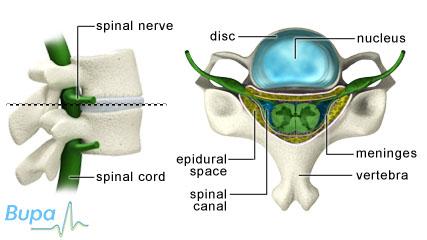
Your back has many interconnecting structures, including bones, joints, muscles, ligaments and tendons. Its main support structure is the spine, which is made up of 24 separate bones called vertebrae, plus the bones of the sacrum and coccyx. Between the vertebrae are discs that act as shock absorbers and allow your spine to bend. Your spinal cord threads down through the central canal of each vertebra, carrying nerves from your brain to the rest of your body.
It’s often very difficult to know exactly what causes back pain, but it’s usually thought to be related to a strain in one of the interconnecting structures in your back, rather than a nerve problem. Back pain caused by a more serious, underlying condition is rare and you’re unlikely to be affected unless you are very old or very young.
Symptoms of back pain
If you have low back pain, you may have tension, soreness or stiffness in your lower back area. This pain is often referred to as ‘non-specific’ back pain and usually improves on its own within a few days.
Back pain may be called either ‘acute’ or ‘chronic’ depending on how long your symptoms last. You may have:
- acute back pain – lasting less than six weeks
- sub-acute back pain – lasting six weeks to three months
- chronic back pain – lasting longer than three months
You should see your GP as soon as possible if, as well as back pain, you have:
- a fever (high temperature)
- redness or swelling on your back
- pain down your legs and below your knees
- numbness or weakness in one or both legs or around your buttocks
- loss of bladder or bowel control (incontinence)
- constant pain, particularly at night
- pain that is getting much worse and is spreading up your spine
These symptoms are known as red flags. It’s important to seek medical help for these symptoms to ensure you don’t have a more serious, underlying cause for your back pain.
Causes of back pain
For most people with back pain, there isn’t any specific, underlying problem or condition that can be identified as the cause of the pain. However, there are a number of factors that can increase your risk of developing back pain, or aggravate it once you have it. These include:
- standing, sitting or bending down for long periods
- lifting, carrying, pushing or pulling loads that are too heavy, or going about these tasks in the wrong way
- having a trip or a fall
- being stressed or anxious
- being overweight
- having poor posture
There may be other, more serious underlying causes of your low back pain, but these are rare. They include:
- fracture – a crack or break in one of the bones in your back
- osteoporosis – a condition where bones lose density causing them to become weak, brittle and more likely to break
- a slipped disc – this is when a disc bulges so far out that it puts pressure on your spinal nerves
- spinal stenosis – a condition in which the spaces in your spine narrow
- spondylolithesis – when one of your back bones slips forward and out of position
- degenerative disc disease – when the discs in your spinal cord gradually become worn down
- osteoarthritis – a wear-and-tear disease that can particularly affect the joints of your spine
- rheumatoid arthritis – an inflammatory condition in which your immune system causes inflammation of the lining of your joints and surrounding structures
Low back pain may also be caused by an infection or cancer, but these two causes are very rare.
Diagnosis of back pain
Your GP will usually be able to diagnose low back pain from your symptoms and there will be no need for further tests. If, however, your symptoms don’t improve after a few weeks, or you have some red flag symptoms, he or she may refer you to a back clinic to have:
- an X-ray
- a CT scan (a test that uses X-ray equipment and computer software to create pictures of the inside of your body)
- an MRI scan (a test that uses magnets and radiowaves to produce images of the inside of the body)
- blood tests
These tests are used to find out if you have a more specific, underlying cause for your back pain.
Treatment of back pain
If your back pain is non-specific, your GP will recommend you try self-help measures. Alternatively, he or she may prescribe medicines or refer you for physical therapy if your pain is severe or chronic. If, however, your GP suspects you have a specific underlying cause, he or she may refer you to a back clinic or a pain clinic to see if you are suitable to have spinal injections. These are used to find out the exact source of, and also to treat, your back pain but aren’t suitable for everyone.
Self-help
There are a number of things you can do to help relieve low back pain.
- Stay active and continue your daily activities as normally as you can. Bed rest may actually make low back pain worse, so try to limit the time you spend resting to a minimum.
- Apply hot or cold packs to the affected area. You can buy specially designed hot and cold packs from most pharmacies. If you prefer, you can apply a cold compress, such as ice or a bag of frozen peas, wrapped in a towel. Don’t apply ice directly to your skin as it can damage your skin.
Medicines
Taking an over-the-counter painkiller (such as aspirin or paracetamol) or anti-inflammatory medicine (such as ibuprofen) is often enough to relieve acute low back pain. You can also use creams, lotions and gels that contain painkillers or anti-inflammatory ingredients. Always read the patient information that comes with your medicine and if you have any questions, ask your pharmacist for advice.
If your pain is severe or chronic, your GP may prescribe stronger medicines such as diazepam, morphine or tramadol. However, these aren’t suitable for everyone because they can be addictive and cause side-effects. Always ask your doctor for advice and read the patient information leaflet that comes with your medicine.
Physical therapies
A physiotherapist (a health professional who specialises in maintaining and improving movement and mobility) may be able to help you design a programme to help you exercise and stretch.
Alternatively, your GP may refer you for physical therapy such as physiotherapy, chiropractic treatment or osteopathy (therapies that are given alongside conventional treatments) to help with your back pain. Treatment can involve exercises, posture advice, massage, and techniques known as spinal mobilisation and spinal manipulation. Treatment courses usually last about six to 12 weeks.
Surgery
Back pain, even if it’s chronic, can usually be treated or managed successfully, but about one in 10 people have ongoing problems. Back surgery is really only considered as a last resort if the pain is related to a specific cause.
Complementary therapies
Some people find acupuncture can help relieve low back pain. You may be able to have a course of up to 10 sessions over a 12-week period.
Alternatively, you could try a pain-management programme to help you better deal with and manage your symptoms.
You should always talk to your GP before trying any complementary therapy.
Prevention of back pain
Good back care can greatly reduce your risk of getting low back pain. To look after your back, make sure you:
- take regular exercise – walking and swimming are particularly beneficial
- try to keep your stress levels to a minimum
- bend from your knees and hips, not your back
- maintain good posture – keep your shoulders back and don't slouch
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email.
I do a lot of lifting and carrying at work. How can I prevent back injury in the workplace?
I have seen many different kinds of mattresses, back supports and insoles advertised for sale. Are any of these effective at preventing or curing back pain?
What are pain-management programmes for back pain?
When I have back pain, I just want to lie down. Why is it important to keep active?
Are there any easy and safe exercises I can do to help relieve my back pain or prevent it returning?
I do a lot of lifting and carrying at work. How can I prevent back injury in the workplace?
There are a number of things you can do to help prevent back injury from lifting and carrying. Always try to think and plan things through before you attempt any strenuous activities.
Explanation
Lifting objects (also known as manual handling) is often part of our daily life and can be a common cause of back pain. Workplace activities that are known to cause or aggravate back pain include:
- stooping, bending over or crouching
- lifting, pushing or pulling bulky, heavy or awkward objects
- stretching, twisting and reaching
- spending prolonged periods in one position, leading to postural strain
- jobs in which your whole body is subjected to vibration, jolting and jarring (such as drilling)
In order to prevent back pain caused by lifting and carrying, it may be helpful to:
- stretch your back before lifting heavy objects
- always bend from your knees, not your back
- turn using your whole body; don't twist your back
- carry objects close to your body
- not carry too many things at once
- ask someone to help you lift particularly heavy objects
- use mechanical handling equipment to lift things for you whenever possible
As a general rule, it’s best to lift with care and not to lift more than you can easily handle. Always think before doing.
If you have back pain and have been off work, it's important to try to get back to work as quickly as possible as this may actually help your recovery. Talk to your employer about making a gradual return to work and whether your duties can be adapted to prevent further back injury.
Also, if your job involves a lot of lifting, you can attend a lifting and manual handling course. These are usually offered by most large employers.
Further information
- BackCare
0845 130 2704
www.backcare.org.uk
- Health and Safety Executive
Sources
- About back pain. BackCare. www.backcare.org.uk, accessed 17 August 2010
I have seen many different kinds of mattresses, back supports and insoles advertised for sale. Are any of these effective at preventing or curing back pain?
There are a number of support aids available for people with back problems. Some of these can be useful, others are of no benefit and some may even do more harm than good. You shouldn’t use any products to try and treat your back pain until you have talked to your GP or an occupational therapist (a health professional who can give practical assistance to help you manage with everyday tasks and increase your independence).
Explanation
The following are examples of different support aids available.
- Medium-firm mattresses. Ideally, your mattress should be soft enough to support and conform to your body shape, yet firm enough to allow you to turn from side to side easily, without twisting your back. Evidence suggests that a medium-firm mattress may give better support than a firm surface for people with chronic low back pain.
- Back supports, corsets and braces. Some people use these when driving or sitting for long periods of time. Evidence suggests, however, that these types of aid may not provide any benefit to people with chronic low back pain. As different types of support are used for different types and causes of back pain, it’s important to remember that using the wrong type might actually make your back pain worse.
- ·Insoles. These are support aids that people place in their shoes to help with their posture. There is limited evidence to show that using insoles will prevent or treat back pain.
Further information
- BackCare
0845 130 2704
www.backcare.org.uk
Sources
- Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 2007; 146:478–91
- van Duijvenbode I, Jellema P, van Poppel M, et al. Lumbar supports for prevention and treatment of low back pain. Cochrane Database of Systematic Reviews 2010, Issue 2. doi:10.1002/14651858.CD001823.pub3.
- Sahar T, Cohen MJ, Ne’eman V, et al. Insoles for prevention and treatment of back pain. Cochrane Database of Systematic Reviews 2007, Issue 4. doi:10.1002/14651858.CD005275.pub2
What are pain-management programmes for back pain?
Your GP may recommend you try a pain-management programme if you have lived with persistent back pain for some time. You can attend a pain clinic or, if you prefer, get in contact with a self-help group.
Explanation
If you have non-specific, ongoing low back pain, a pain-management programme may be able to help you find ways of controlling and living with your symptoms. Exercising and regaining your physical confidence are important parts of the pain-management approach, as are learning about the physical and psychological factors that contribute to pain.
Pain-management programmes are usually provided as an outpatient service. You may attend the sessions with a group of people and will be led by a team of health professionals, including a physiotherapist.
Alternatively, you may decide to try a self-help group who can provide further support and information.
Further information
- BackCare
0845 130 2704
www.backcare.org.uk
- British Pain Society
Sources
- Back pain. Arthritis Research UK. www.arthritisresearchuk.org, accessed 17 August 2010
When I have back pain, I just want to lie down. Why is it important to keep active?
There is clear evidence that bed rest or being inactive won’t help back pain.
Explanation
It was once thought that staying in bed would ease a painful back. Now the advice is to keep as active as you can and get back to your normal activities as soon as possible. Evidence shows that staying in bed can cause your joints to stiffen, your muscles to lose strength and generally cause you to take longer to recover. Staying active can reduce the time you need off work and can reduce the chances of ongoing, chronic problems.
Further information
-
BackCare
0845 130 2704
www.backcare.org.uk
Sources
- About back pain. BackCare. www.backcare.org.uk, accessed 17 August 2010
- Dahm KT, Brurberg KG, Jamtvedt G, et al. Advice to rest in bed versus advice to stay active for acute low-back pain and sciatica. Cochrane Database of Systematic Reviews 2010, Issue 6. doi:10.1002/14651858.CD007612.pub2
Are there any easy and safe exercises I can do to help relieve my back pain or prevent it returning?
Yes. Doing regular exercise can help to reduce and relieve your back pain, and even prevent it from returning. Always speak to your GP or physiotherapist before starting a new exercise programme.
Explanation
There’s a whole range of physical activities you can take part in to keep your back healthy. Research suggests it may help if you have back pain that lasts for longer than six weeks. You may be able to try:
- walking, jogging or running
- yoga, pilates or tai chi
- swimming
- cycling
- hydrotherapy (exercises in water)
Always remember to speak to your GP or physiotherapist before starting a new training programme, especially if you haven’t done any regular physical activity for some time.
Further information
- BackCare
0845 130 2704
www.backcare.org.uk
Sources
- About back pain. BackCare. www.backcare.org.uk, accessed 17 August 2010
- Hayden J, van Tulder MW, Malmivaara A, et al. Exercise therapy for treatment of non-specific low back pain. Cochrane Database of Systematic Reviews 2005, Issue 3. doi:10.1002/14651858.CD000335.pub2
Related topics
Acupuncture
Back surgery
Chiropractic
Discography
Osteopathy
Osteoarthritis
Osteoporosis
Over-the-counter painkillers
Rheumatoid arthritis
Spinal injections for chronic low back pain
Further information
-
BackCare
0845 130 2704
www.backcare.org.uk -
Chartered Society of Physiotherapy
www.csp.org.uk -
General Osteopathic Council
www.osteopathy.org.uk -
General Chiropractic Council
www.gcc-uk.org
Sources
- Back pain. Arthritis Research UK. www.arthritisresearchuk.org, accessed 17 August 2010
- About back pain. BackCare. www.backcare.org.uk, accessed 17 August 2010
- Back pain – low (without radiculopathy). Clinical Knowledge Summaries. www.cks.nhs.uk, published November 2009
- Musculoskeletal lower back pain. Best Practice. http://bestpractice.bmj.com, accessed 24 August 2010
- Low back pain: Early management of persistent non-specific low back pain. National Institute for Health and Clinical Excellence (NICE). May 2009. http://guidance.nice.org.uk/CG88
- Furlan AD, Imamura M, Dryden T, et al. Massage for low-back pain. Cochrane Database of Systematic Reviews 2010, Issue 4. doi:10.1002/14651858.CD001929.pub2
- Furlan AD, van Tulder MW, Cherkin D, et al. Acupuncture and dry-needling for low back pain. Cochrane Database of Systematic Reviews 2005, Issue 1. doi:10.1002/14651858.CD001351.pub2
- Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: A joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 2007; 146:478–91
- van Duijvenbode I, Jellema P, van Poppel M, et al. Lumbar supports for prevention and treatment of low back pain. Cochrane Database of Systematic Reviews 2010, Issue 2. doi:10.1002/14651858.CD001823.pub3.
- Sahar T, Cohen MJ, Ne’eman V, et al. Insoles for prevention and treatment of back pain. Cochrane Database of Systematic Reviews 2007, Issue 4. doi:10.1002/14651858.CD005275.pub2
- Dahm KT, Brurberg KG, Jamtvedt G, et al. Advice to rest in bed versus advice to stay active for acute low-back pain and sciatica. Cochrane Database of Systematic Reviews 2010, Issue 6. doi:10.1002/14651858.CD007612.pub2
- Hayden J, van Tulder MW, Malmivaara A, et al. Exercise therapy for treatment of non-specific low back pain. Cochrane Database of Systematic Reviews 2005, Issue 3. doi:10.1002/14651858.CD000335.pub2
This information was published by Bupa’s Health Information Team and is based on reputable sources of medical evidence. It has been peer reviewed by Bupa doctors. The content is intended for general information only and does not replace the need for personal advice form a qualified health professional.
Publication date: October 2010















