Childhood immunisations
Immunisation (also called vaccination) is the use of vaccines to protect your child against infectious diseases.
About childhood immunisations
Why immunise?
Vaccines offered in the UK
Vaccines explained
UK immunisation schedule
How are vaccines given?
When to delay immunisation
Side-effects of immunisations
Are vaccines safe?
About childhood immunisations
Babies are born with some immunity to infectious diseases such as measles. This ‘passive immunity’ is passed on from mother to baby, but it only lasts for a few months. Your child will need to develop his or her own antibodies (proteins produced by the immune system) to fight against bacteria and viruses.
Vaccines stimulate the immune system in the same way as an infection, but without causing a full-blown disease. Vaccines are a safe way to ensure your child develops his or her own antibodies to a particular infection. Vaccines are made using:
- dead viruses or bacteria
- inactivated toxin from a virus or bacterium
- a weakened form of a live virus or bacterium (called a live vaccine)
- parts of a virus or bacterium, but not the whole organism (called component vaccine)
Why immunise?
All of the infections that are in the immunisation programme can develop into serious illness, and have the potential to cause disability or death. Vaccinating your child means he or she is protected from these serious illnesses and their potentially devastating effects.
If most children are immunised, then the risk of infection in the community is significantly reduced and even unvaccinated children are at much less risk of catching the illness. This is called ‘herd immunity’. For example, if nine out of 10 children have the measles, mumps and rubella (MMR) vaccine, these diseases may be eliminated from the community.
Some people argue that there is no longer any need to immunise children. Diseases such as polio, for example, are now almost never seen in the UK. However, these diseases haven’t yet disappeared and if your child comes into contact with someone with the disease, either in the UK or abroad, then he or she is likely to catch it. For example, paralysis from polio still occurs all over the world. If more people choose not to immunise their children, then the number of children at risk of catching a disease will increase and outbreaks of the disease will occur.
The only time to stop immunising children is when a disease has been completely eradicated worldwide as, for example, smallpox was in 1979.
Vaccines offered in the UK
Vaccines given routinely to children in the UK protect against:
- diphtheria
- tetanus
- pertussis (whooping cough)
- polio
- Haemophilus influenzae type B (Hib)
- meningitis C
- pneumococcal infection (eg pneumonia, septicaemia and meningitis)
- measles
- mumps
- rubella (German measles)
- human papilloma virus (HPV)
The following vaccines are given selectively:
- Bacille Calamette Guerin (BCG) – protects against tuberculosis (TB)
- hepatitis B
For some immunisations, your baby will need a course of vaccines to build up his or her defences. Booster vaccines are needed to ‘top up’ immunity for pre-school children and teenagers.
Vaccines explained
DTaP/IPV/Hib vaccine
The DTaP/IPV/Hib vaccine is a combined five-in-one treatment against the following diseases.
- D – diphtheria
- T – tetanus
- aP – acellular pertussis (whooping cough)
- IPV – polio
- Hib – Haemophilus influenzae type B
Pneumococcal vaccine (PCV)
PCV protects against some strains of pneumococcal infection, which can cause diseases such as pneumonia, septicaemia and meningitis.
Meningococcus type C (Men C) vaccine
The Men C vaccine protects against the bacterium that causes a severe form of blood poisoning (septicaemia) and/or meningitis. Your child can have it at the same time as the DTaP/IPV/Hib vaccine. It is given as a separate injection.
Measles/mumps/rubella (MMR) vaccine
The MMR vaccine protects against measles, mumps and rubella.
Bacille Calamette Guerin (BCG) vaccine
The BCG vaccine protects against TB. BCG vaccination is usually given only to those children who are most likely to catch the disease, such as:
- children living in areas with a high rate of TB
- children whose parents or grandparents were born in a country with a high rate of TB
Your child will have a skin test before the injection and then, if needed, he or she will have one injection in the upper arm.
Hepatitis B vaccine
Hepatitis B vaccine is usually given only to those children who are most likely to catch the disease, such as those who have a parent with hepatitis B.
Human papilloma virus (HPV) vaccine
Girls aged 12 to 13 are now routinely given the HPV vaccine. It protects against the two main viruses that cause cervical cancer.
UK immunisation schedule
The following table shows when to immunise your child against each disease.
| Age | Vaccine | Type of injection | Stage of vaccine course |
| 2 months | DTaP/IPV/Hib | 5-in-1 | First dose |
| PCV | Single | First dose | |
| 3 months | DTaP/IPV/Hib | 5-in-1 | Second dose |
| Men C | Single | First dose | |
| 4 months | DTaP/IPV/Hib | 5-in-1 | Third dose |
| Men C | Single | Second dose | |
| PCV | Single | Second dose | |
| 12 months | Hib/Men C | Single | Booster |
| 13 months | MMR | 3-in-1 | First dose |
| PCV | Single | Booster | |
| 3 years and 4 months to 5 years | MMR | 3-in-1 | Booster |
| DTaP/IPV | 4-in-1 | Booster | |
| 12 to 13 years (girls) | HPV | Single | Three doses given over six months |
| 13 to 18 years | Td/IPV | Single | Booster |
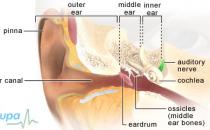
How are vaccines given?
Vaccines are given by injection, usually into the muscle in the upper arm or thigh.
When to delay immunisation
If your child is in good health and due for a vaccine you shouldn’t delay having the immunisation.
A vaccine won’t be given if your child has a fever at the time the injection is due. The vaccine could increase the fever and also your child’s current illness could make it difficult to identify any side-effects to the vaccine. Your GP or nurse will usually examine your child and re-arrange the appointment if your child is too unwell to have the injection.
If you have any concerns about a particular vaccine or if your child has an egg allergy, talk to your GP, practice nurse or health visitor.
Your child won’t be given live vaccines, such as MMR and BCG, if he or she:
- is being treated for cancer, or has been treated for cancer in the last six months
- has a weak immune system
- is taking medicines to suppress his or her immune system
- has had a bone marrow transplant in the last six months
- is taking a course of steroids, for example for asthma
Speak to your GP if your child has any condition affecting his or her immune system.
Incorrect reasons to delay immunisation
Don’t delay getting your child immunised if he or she:
- has a minor illness, such as a cough or cold
- has already had an illness similar to that covered by a combined vaccine (for example, if your child has had mumps, he or she should still have the MMR vaccine)
- is being treated with antibiotics, topical steroids or replacement corticosteroids
- was a premature or very small baby, or jaundiced after birth
- is being breastfed or if the mother is pregnant
- has a stable neurological condition, such as cerebral palsy
- has asthma, hay fever or eczema
- is due to have or has recently had surgery
- is over the immunisation age recommended in the schedule
- has a family history of side-effects to a vaccine, inflammatory bowel disease or autism
- has food allergies, inflammatory bowel disease or autism
Side-effects of immunisations
Side-effects are the unwanted but mostly mild and temporary effects of a successful immunisation. Side-effects of a vaccine may include:
- some redness and swelling at the injection site
- a raised temperature (above 37.5°C but below 39°C)
- sickness and/or diarrhoea
- swollen glands
- a small lump at the injection site, which may last a few weeks
- irritability
You can help to lower your child’s temperature and relieve any discomfort by:
- giving your child liquid paracetamol, such as Calpol – always read the patient information that comes with the medicine and if you have any questions, ask your pharmacist for advice
- removing some clothes and blankets
- sponging him or her with lukewarm water and allowing it to dry on the skin
Severe reactions
A severe reaction to a vaccine is very rare. You should seek urgent medical attention if your child has any of the following symptoms.
- A very high temperature (over 39°C).
- A fit – this is called a febrile convulsion.
- A rash.
- Difficulty with breathing.
- Floppiness or lethargy.
- Inconsolable crying which may be high-pitched and unusual.
Are vaccines safe?
Health professionals recognise that routine immunisation is the best defence against potentially dangerous diseases and it is a safe way to ensure protection. There have been some controversies and speculations over certain vaccines in recent years.
- The use of mercury-based preservative thiomersal in the manufacture of vaccines. Purely as a precaution, and a general move to reduce children’s exposure to mercury, thiomersal has been removed from vaccines. None of the routine childhood vaccines contain any thiomersal.
- MMR vaccine and autism. Research studies show there is no link between MMR and autism.
- In 2010, the media reported a possible link between HPV vaccine and a death of a schoolgirl. Subsequent investigation showed no link and the death was due to an unrelated illness.
Answers to questions about childhood immunisation
What happens if my child misses his or her booster dose of a vaccine?
Can my baby’s immune system cope with receiving so many vaccines all at once?
If my child is ill, will he or she still be able to respond to a vaccine?
Why are girls being offered the cervical cancer vaccine at such a young age?
What happens if my child misses his or her booster dose of a vaccine?
Your child won’t be fully protected if he or she hasn’t received all the doses of a vaccine.
Explanation
There are two major reasons for booster doses: to protect your child and to protect the entire population of children.
First, booster doses ‘top up’ the level of antibodies produced by your child in response to the particular vaccine. If your child hasn’t received all the doses, his or her level of protection will be reduced.
Secondly, having a high level of immunity among the general population (herd immunity) is vital to reduce the risk of spread of disease from person to person. The lower the herd immunity – the greater the risk of a having a disease outbreak.
If your child has missed an appointment and is late getting a booster dose, just make an appointment as soon as possible. The gap that’s advised you should leave between having a vaccine and having the booster dose is the ideal amount of time – but the booster will still work if it’s given later. You won’t have to start the course of vaccines again.
Can my baby’s immune system cope with receiving so many vaccines all at once?
Yes. The vaccines can’t cause a full-blown illnesses, which means your baby’s immune system can easily cope with them.
Explanation
Some parents worry about the number of vaccines children receive these days. However, it has been estimated that a baby’s immune system could respond to as many as 10,000 vaccines at any one time.
A vaccine doesn’t ‘weaken’ the immune system or put your child at higher risk of having other infections while his or her immune system is responding to the vaccine.
If my child is ill, will he or she still be able to respond to a vaccine?
Yes, having an illness doesn’t reduce your child's ability to respond to a vaccine.
Explanation
It’s a common misconception that children who are ill will be less likely to respond to a vaccine, or more likely to get side-effects, as their immune system is compromised.
Parents may also wrongly believe that giving a vaccine to a child who is ill may burden the immune system, at a time when the child is already trying to fight off an infection.
The response to a vaccine is the same in healthy children and those with mild or moderate illness. However, if your child is feeling unwell, your doctor or nurse will usually suggest postponing the immunisation until the child is fully recovered. This isn’t done because your child may not respond well to the vaccine, but to ensure that symptoms of your child’s current illness are not mistaken as side-effects of the vaccine.
Also, a common side-effect to any vaccine is a high temperature. If your child has a high temperature or fever at the time the injection is due, the vaccine is often delayed to avoid making it worse.
Why are girls being offered the cervical cancer vaccine at such a young age?
The cervical cancer vaccine is most effective when it’s given before a girl becomes sexually active.
Explanation
The HPV vaccine protects you against two specific types of HPV, which are the most likely to cause cervical cancer. These are HPV types 16 and 18, which cause around seven out of 10 cases of cervical cancer. The vaccine doesn’t provide protection against any other types of HPV.
The HPV vaccine is given to girls aged 12 and 13. This is because the vaccine is more effective if it’s given to girls before they become sexually active. There is another HPV vaccine which also offers protection against genital warts but it is not available on the NHS.
Further information
-
NHS immunisation information
www.immunisation.nhs.uk
Sources
- About immunisation. NHS Immunisation Information. www.immunisation.nhs.uk, accessed 21 April 2010
- The vaccines. NHS Immunisation Information. www.immunisation.nhs.uk, accessed 21 April 2010
- FAQs. NHS Immunisation Information. www.immunisation.nhs.uk, accessed 21 April 2010
- The Green Book, Chapter 11: Immunisation schedule. Department of Health, 2006. www.dh.gov.uk
- The Green Book, Chapter 6: Vaccine safety and the management of adverse events following immunisation. Department of Health, 2008. www.dh.gov.uk
- Immunizations. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 26 February 2010
Related topics
- MMR vaccine
- The HPV vaccine