Gout
Published by Bupa's Health Information Team, May 2010.
This factsheet is for people who have gout, or who would like information about it.
Gout is a condition that causes swelling and pain in joints, usually in the arms or legs.
About gout
Symptoms of gout
Complications of gout
Causes of gout
Diagnosis of gout
Treatment of gout
Prevention of gout
About gout
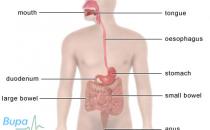
Gout is an arthritic condition, meaning that it causes inflammation of your joints. It causes pain and swelling, usually in one joint in your body – commonly your big toe. However, it can affect any of your joints, including those in your:
- heels
- insteps (arches of your feet)
- ankles
- knees
- fingers
- wrists
- elbows
According to the UK Gout Society, gout affects around one in every 100 people. It’s more common in men, particularly those aged 30 to 60, and in older people.
Symptoms of gout
The symptoms of gout include:
- severe pain in your joint
- swelling and warmth around your joint
- red and shiny skin around your joint
- mild fever
- firm, white lumps beneath your skin – these are urate crystals called tophi
If you have these symptoms, see your GP.
You will usually have gout for a period of up to two weeks (an attack) and then it will go away, even without treatment. With treatment, this can be reduced to less than a week. You may only ever have one attack of gout in your lifetime, but for many people it returns.
Complications of gout
It's uncommon for gout to cause any further problems but you may develop:
- gout affecting several of your joints (called polyarticular gout)
- inflamed tophi, which can cause discomfort
- kidney stones (if urate crystals collect in your urinary tract)
- kidney damage (if urate crystals collect in your kidney tissue)
Causes of gout
You can develop gout if you have too much urate in your body. Urate (also called uric acid) is a chemical that everyone has in their blood. It’s a waste product formed from substances called purines, which are found in every cell in your body and certain foods. Excess urate is usually passed through your kidneys and out of your body in your urine. However, the level of urate in your blood can rise if:
- your kidneys don't pass urate quickly enough
- your body produces too much urate
If the level of urate in your body is too high, it can form tiny crystals that collect in your tissues, particularly in and around your joints. This is what causes the swelling and pain. These crystals form at cooler temperatures, which is why gout is common in your fingers and toes.
Not everybody with high levels of urate gets gout and some people get gout but don't have high levels of urate. It's not known why some people develop gout and others don't. However, there are certain factors that can increase your likelihood of getting gout. You’re more likely to have gout if you:
- are a man aged 30 to 60
- are a woman who has been through the menopause, although women are much less likely to develop gout than men
- eat a diet that contains high levels of purines, which are commonly found in red meat and seafood – urate is formed in your body when the purines in foods you eat and old cells in your body are broken down
- drink too much alcohol
- take certain medicines, such as diuretics (‘water tablets’), which increase the flow of urine from your body
- have a family history of gout
- have kidney disease meaning that your kidneys don’t pass enough urate out in your urine
- are overweight
- have a medical condition such as psoriasis (itchy, dry and flaky skin) which can sometimes cause your body to produce too much urate
- have high blood pressure
- injure a joint
- are taking certain types of cancer medicines
An attack of gout often occurs for no clear reason, but may be triggered by an illness, injury or drinking too much alcohol.
Diagnosis of gout
Your GP will ask about your symptoms and examine you. He or she will usually take a sample of your blood, which will be sent to a laboratory to measure the levels of urate.
Your GP may refer you to a rheumatologist (a doctor specialising in conditions that affect the joints) for further tests.
Your doctor may remove some fluid from your swollen joint with a needle. This usually causes no more discomfort than a blood test. If urate crystals can be seen in the fluid under a microscope, you have gout. If calcium crystals are seen, you have a similar condition called pseudogout. The crystals formed when you have pseudogout aren’t urate crystals – they are made of a calcium salt called calcium pyrophosphate.
You may need to have an X-ray taken of your joint in order to rule out other conditions, but this is less common.
Treatment of gout
Self-help
There are a number of steps you can take to reduce the pain and swelling of a gout attack. Left untreated, attacks of gout may become more frequent and last for longer.
- Raise and rest your joint. You shouldn't do any vigorous physical activity. Sometimes your doctor may give you a splint to wear to stop you moving your joint.
- Keep your joint cool and don't cover it. Apply ice wrapped in a towel to your joint for about 20 minutes to help reduce swelling. You shouldn't apply ice directly to your skin as it can damage your skin. If you need to repeat this, let your joint return to its normal temperature first.
Medicines
There are some medicines your doctor can prescribe to help ease the pain and swelling of an attack of gout.
Non-steroidal anti-inflammatory drugs (NSAIDs), such as naproxen, may relieve pain and inflammation. If you have a heart condition, high blood pressure, kidney disease, lung disease or if you’re over 65, these medicines may be harmful so you should talk to your doctor about taking them.
If NSAIDs aren't suitable for you, your doctor may prescribe a medicine called colchicine as an alternative. Colchicine works by reducing the build-up of urate in your body. It can have side-effects including sickness and diarrhoea.
Occasionally, your doctor may prescribe steroid tablets if you can't take NSAIDs or colchicine. Alternatively, your doctor may recommend a steroid injection if you have gout in a large joint (such as your knee).
If you have repeat attacks of gout, there are medicines you can take to help to prevent it.
Your doctor may prescribe a medicine called allopurinol for you to take daily. This medicine prevents gout by stopping the formation of urate. Allopurinol may actually cause an attack of gout when you first start taking it. This is because the level of urate in your body will rise a bit before it falls. To help prevent this happening, your doctor may prescribe NSAIDs, colchicine or steroid tablets for you to take alongside allopurinol for up to three months. Make sure you drink enough fluids when taking these medicines.
Your doctor may prescribe a medicine such as probenecid or sulphinpyrazone to increase the amount of urate that is removed from your body in your urine. These medicines aren't used to treat an acute attack of gout and are usually prescribed once an attack is over.
Always ask your doctor for advice and read the patient information leaflet that comes with your medicine.
Prevention of gout
Identifying anything that brings on an attack of gout and not doing these things is very important.
For example, you:
- shouldn't eat foods that are very high in purines, such as liver, kidney and seafood (especially oily fish such as mackerel, sardines and anchovies), and certain vegetables (asparagus, cauliflower, lentils, mushrooms, oatmeal and spinach) – ask your doctor or a dietician for more advice
- shouldn't drink too much alcohol – especially beer, stout, port and fortified wines
- should eat a well-balanced diet and do regular physical activity to lose excess weight
- should drink enough water
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email.
I’ve been diagnosed with gout. Are there any foods I should avoid?
I've been diagnosed with pseudogout. What's the difference between that and ‘real’ gout?
I’ve heard that fizzy drinks can cause gout. Is that true?
I have had a few attacks of gout and I am now taking allopurinol. Can I expect any serious side-effects?
I've been diagnosed with gout. Are there any foods I should avoid?
You shouldn’t eat foods that contain very high levels of purines. Purines are substances that are broken down into urates and can make gout worse. Foods that contain high levels of purines include certain meats, seafood and pulses.
Explanation
Gout is caused by a build up of urates (uric acid), a waste product formed from purines (which are found in every cell in your body and certain foods). Your diet plays an important role in causing gout and increasing your risk of further attacks.
If you have gout, you shouldn’t eat too many foods that are very high in purines. These foods include:
- meats, such as red meat and offal (eg liver and kidneys)
- game (eg pheasant and rabbit)
- seafood (shellfish including mussels and shrimp and oily fish such as sardines and herring)
- yeast-containing food and drink, such as Marmite and beer
- mushrooms and foods made from mushrooms (eg Quorn)
- certain vegetables (eg cauliflower, asparagus and spinach)
- beans and pulses (eg lentils)
You don’t have to cut out all of these foods completely as they may contain other essential nutrients (for example, protein and iron in red meat), but you should cut down on how much of them you eat. Instead, you should eat more sources of protein that are low in purines, such as milk, cheese and eggs.
Some people find that other foods make their gout worse. These can include strawberries, oranges and tomatoes. If these foods affect you, it’s probably best to avoid them. If you have gout, you should also cut down on how much alcohol you drink.
Further information
Arthritis Research Campaign
0870 850 5000
www.arc.org.uk
UK Gout Society
www.ukgoutsociety.org
Sources
- All about gout and diet. UK Gout Society. www.ukgoutsociety.org, accessed 17 March 2010.
I've been diagnosed with pseudogout. What's the difference between that and ‘real’ gout?
You’re diagnosed with pseudogout when the pain and swelling in your joint is caused by different crystals to the ones that cause ‘real’ gout.
Explanation
You can develop gout if you have too much urate in your body. Urate (also called uric acid) is a chemical that everybody has in their blood. If the level of urate in your body is too high, it can form tiny crystals that collect in your tissues, particularly in and around your joints. This is what causes the swelling and pain.
The crystals formed when you have pseudogout aren’t urate crystals, as they are with ‘real’ gout. They are made of a calcium salt called calcium pyrophosphate.
Pseudogout is most common in people over 65. Any joint can be affected, but it's usually your knee. An attack of pseudogout usually starts with severe pain, stiffness and swelling and settles on its own, getting better within three weeks. Sometimes another illness can set off an attack of pseudogout, but often there is no apparent reason for one starting.
If you think you may have gout or pseudogout, contact your GP for advice.
Further information
Arthritis Research Campaign
0870 850 5000
www.arc.org.uk
UK Gout Society
www.ukgoutsociety.org
Sources
- Calcium crystal diseases (pseudogout). Arthritis Research UK. www.arthritisresearchuk.org, accessed 17 March 2010
I have had a few attacks of gout and I’m now taking allopurinol. Can I expect any serious side-effects?
In general allopurinol has no serious side-effects, but when you take any medicine you should look out for anything unusual and see your GP if you’re worried.
Explanation
Allopurinol is a medicine that prevents gout by stopping the formation of urate.
You may get an attack of gout during the first few months after you first start taking allopurinol. This is because the level of urate in your body will rise a bit before it falls. Your GP or rheumatologist (doctor who specialises in conditions that affect the joints) may prescribe you a non-steroidal anti-inflammatory (NSAID) medicine or a medicine called colchicine to take alongside allopurinol to try to prevent this.
People have occasionally developed a rash after taking allopurinol. If you have a rash, you should contact your GP or your rheumatologist as soon as possible
It's unusual to have any serious side-effects with allopurinol. However, if you’re worried about anything unusual when you’re taking allopurinol, contact your doctor.
Further information
Arthritis Research Campaign
0870 850 5000
www.arc.org.uk
UK Gout Society
www.ukgoutsociety.org
Sources
- Joint Formulary Committee, British National Formulary. 58th ed. London: British Medical Association and Royal Pharmaceutical Society of Great Britain, 2009: 581-82
Related topics
Non-steroidal anti-inflammatory drugs (NSAIDs)
This information was published by Bupa's Health Information Team and is based on reputable sources of medical evidence. It has been peer reviewed by Bupa doctors. The content is intended for general information only and doesn’t replace the need for personal advice from a qualified health professional.
Publication date: May 2010.
Gout factsheet
Visit the gout health factsheet for more information.
Related topics
Alcohol – sensible drinking
Chemotherapy
Diuretics
Healthy eating
Healthy weight for adults
High blood pressure
Kidney stones
Non-steroidal anti-inflammatory drugs (NSAIDs)
Psoriasis
Sensible drinking
X-ray
Further information
Arthritis Research Campaign
0870 850 5000
www.arc.org.uk
British Society for Rheumatology
020 7842 0900
www.rheumatology.org.uk
UK Gout Society
www.ukgoutsociety.org
Sources
- All about gout. UK Gout Society. www.ukgoutsociety.org, accessed 17 March 2010
- Gout – making a diagnosis: examination. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 17 March 2010
- Gout – background information: prevalence. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 17 March 2010
- Gout. Arthritis Research UK. www.arthritisresearchuk.org, accessed 17 March 2010
- Gout – background information: causes and risk factors. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 17 March 2010
- Gout – making a diagnosis: history. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 17 March 2010.
- All about gout and treatments. UK Gout Society. www.ukgoutsociety.org, accessed 17 March 2010.
- Gout – background information: complications and prognosis. www.cks.nhs.uk, accessed 17 March 2010.
- Gout – management: scenario acute gout: self care. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 17 March 2010.
- All about gout and diet. UK Gout Society. www.ukgoutsociety.org, accessed 17 March 2010
- Joint Formulary Committee, British National Formulary. 58th ed. London: British Medical Association and Royal Pharmaceutical Society of Great Britain, 2009: 581-82
- Calcium crystal diseases (pseudogout). Arthritis Research UK. www.arthritisresearchuk.org, accessed 17 March 2010.
- Simon C, Everitt H, and Kendrick T, Oxford Handbook of General Practice. 3rd ed. Oxford: Oxford University Press, 2010: 528
This information was published by Bupa's Health Information Team and is based on reputable sources of medical evidence. It has been peer reviewed by Bupa doctors. The content is intended for general information only and doesn’t replace the need for personal advice from a qualified health professional.
Publication date: May 2010.