Knee injuries
Knee injuries are common, especially when taking part in sport. Injuries to soft tissues, such as ligaments and tendons, are the most common, though damage to the bones is also possible.
About knee injuries
Symptoms of knee injuries
Causes of knee injuries
Diagnosis of knee injuries
Treatment of knee injuries
Prevention of knee injuries
About knee injuries
The most common knee injuries are:
- a sprain – one or more ligaments is overstretched through twisting or pulling; the ligament may be torn or ruptured
- a strain – a tendon or muscle is overstretched
- damage to the cartilage in your knee – the cartilage is a crescent-shaped disc called a meniscus, that acts as a ‘shock absorber’ in your knee
- overuse – this is most common in people who run
Knee ligament injuries
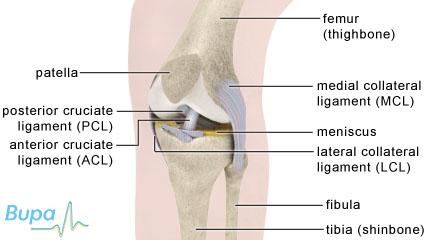
Ligaments connect one bone to another. The ligaments outside your knee joint are called the medial collateral ligament and the lateral collateral ligament. They provide your knee with stability and limit the amount it can move from side to side.
The medial collateral ligament is on the inner side of your knee and is taut when your leg is straight. It's a strong ligament but can be sprained or completely ruptured (torn) if you twist your straightened leg at the same time as being knocked sideways, for example, when being tackled in rugby.
The lateral collateral ligament is like a thin, strong cord that runs on the outer side of your knee connecting the bottom of your thigh bone to the top of your fibula (one of the bones in your lower leg). It's not usually damaged on its own, but you may need to have it repaired if you have damaged other ligaments.
Medial and lateral collateral ligament injuries may be classed as follows:
- grade 1 is a sprain with no tearing of the ligament
- grade 2 is a partial tear of the ligament
- grade 3 is a complete tear of the ligament
The ligaments inside your knee joint are called the anterior cruciate ligament and the posterior cruciate ligament. Cruciate means in the form of a cross – the anterior cruciate ligament crosses over in front of the posterior cruciate ligament. These ligaments provide stability to your knee, when it is in different positions, particularly in the forward and backward movements of the knee joint.
Other soft tissue injuries
The other soft tissues around your knee can also be injured. Soft tissue means any tissue in your body that isn't bone.
If you play a sport that involves twisting your upper leg while your foot is planted on the floor, you may tear the cartilage in your knee. The cartilage becomes worn down (degenerates) as you get older, making it easier to tear even after a very minor injury.
Overuse of your knee can also result in tearing a patellar tendon. Your patellar tendon connects your kneecap (patella) to your thigh muscle.
Symptoms of knee injuries
The symptoms for most ligament injuries will be similar, no matter which one has been damaged. These may include:
- pain
- swelling
- instability – you may feel like your knee is giving way or that it’s locking
You may feel a popping or snapping sensation at the time of the injury, or even hear a popping sound. You may also find that you can’t stand properly on the affected leg, or put your full weight on it.
You won’t feel any direct pain if you injure the cartilage in your knee, but you may have some pain or discomfort from the swelling that follows an injury. Pain may develop on either the inside or outside of your knee joint (depending on which knee you have damaged the cartilage) and you may see some swelling.
If you have any of these symptoms, visit your GP or physiotherapist for advice.
Causes of knee injuries
You may injure your knee if:
it receives an impact or is moved beyond its usual range of movement, for example if you have a fall or land awkwardly
you play a sport that combines running, jumping and stopping with quick changes of direction, such as football
you have a condition such as osteoarthritis or gout, or are very overweight
your knees hit the dashboard in a car accident – posterior cruciate ligament damage is sometimes called the ‘dashboard injury’ as this is often how it occurs
Diagnosis of knee injuries
Your GP or physiotherapist will ask about your symptoms and examine you. This may include feeling for fluid in the joint by pressing gently over your kneecap, especially if your knee doesn’t look severely swollen. Your GP or physiotherapist will ask you to describe how the injury happened, where your pain is and what type of pain it is.
Your GP or physiotherapist may test for injury to your knee ligaments or soft tissues by bending and flexing your knee, and moving your leg into different positions, while you lie or sit down.
Your GP or physiotherapist may also ask you to perform movements such as stepping, squatting or hopping.
Your GP/physiotherapist may refer you for other tests in a hospital or clinic. These may include an MRI or ultrasound scan or occasionally X-ray. These tests can help to diagnose more complicated or severe injuries.
Treatment of knee injuries
The treatment you will receive will depend on what damage you have done and how bad the damage is.
Self help
You should follow the PRICE procedure to manage any type of soft tissue injury to your knee. PRICE stands for the following.
- Protection. Protect your injury from further harm.
- Rest. Rest the injury for the first two to three days, then reintroduce movement so you don't lose too much muscle strength.
- Ice. Apply a cold compress such as ice or a bag of frozen peas wrapped in a towel to help reduce swelling and bruising. Don’t apply ice directly to your skin as it can damage your skin.
- Compression. Compress the joint by bandaging it to support the injury and help decrease swelling.
- Elevation. Elevate your knee by resting it above the level of your heart and keep it supported.
There are certain things you should not do in the first three days after your injury to avoid doing further damage to your knee. These can be remembered as HARM.
- Heat. This includes having a hot bath or using a heat pack.
- Alcohol. Drinking alcohol can increase bleeding and swelling in the affected area.
- Running or other forms of exercise.
- Massaging the injured knee. This can cause more swelling or bleeding.
You may need to use crutches or wear a brace to make sure that you keep weight off the affected knee.
Medicines
You can buy painkillers such as paracetamol or ibuprofen to treat mild and moderate pain. Your GP may prescribe stronger painkillers if your pain is severe. As well as easing your pain, painkillers may help to any reduce inflammation and swelling. Always read the patient information that comes with your medicine and if you have questions, ask your pharmacist or doctor for advice.
Physiotherapy
If your injury is more severe or complex, your GP may refer you to a physiotherapist (a health professional who specialises in movement and mobility). You can also choose to see a physiotherapist privately. He or she will develop a programme of rehabilitation exercises to gradually strengthen your knee and stretch your muscles. These exercises will vary depending on the kind of injury you have and how severe it is. Your physiotherapist may also use various techniques to help speed up the healing of your knee.
Braces to support your knee are occasionally used during rehabilitation, usually when an injury has been severe.
Surgery
In some situations, you may need to have surgery to repair the injury to your knee. This is likely to be the case if:
- you have ruptured your lateral collateral ligament
- you have damaged your anterior cruciate ligament and you do a lot of sport, or have also torn cartilage or your medial collateral ligament – you may need a reconstruction operation, which involves taking a graft of tendon (usually from your kneecap) to replace the damaged ligament
- more than one ligament or tissue in your knee has been damaged
- you have torn your patellar tendon
- your knee remains painful or locks after a meniscus injury
Prevention of knee injuries
There are some precautions you can take to try to reduce the risk of damaging your knee ligaments.
- Exercise regularly to maintain a good level of fitness. This will mean your muscles are stronger and better able to support your joints, including your knees. If you haven’t been active for a while, start gently and gradually increase the intensity.
- Spend five to 10 minutes warming up before exercise to increase blood flow to your muscles and reduce the chance of an injury. Many sports professionals advise stretching your muscles after warming up and again after cooling down; however the benefit of stretching before or after exercise is unproven.
Answers to questions about knee injuries
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email.
I have sprained a ligament in my knee. How long will it take to heal?
Which painkillers are best for a knee injury?
Can I use a gel or spray painkiller directly on my skin instead of tablets? Are these effective?
Can arnica help with my knee injury?
Is a knee injury more likely because I have osteoarthritis?
I have sprained a ligament in my knee. How long will it take to heal?
Answer
The time your sprain will take to heal depends on which part of your knee you have injured and how badly. If it’s a mild sprain, the ligament is likely to heal within three to six weeks. If your injury is more severe and depending on whether you require surgery, full recovery can take between two and 12 months.
Explanation
The most important way to help your injury to heal is to follow the PRICE method immediately after the injury. PRICE means protection, rest, ice, compression and elevation. If your symptoms don't improve or any pain or swelling gets worse, talk to your doctor about physiotherapy or other treatment.
Which painkillers are best for a knee injury?
Answer
Talk to your pharmacist or your GP about the medicines available and which ones are best for you.
Explanation
Paracetamol should give you some pain relief. If paracetamol doesn’t ease your pain, your GP may suggest a stronger painkiller called codeine. You can also use anti-inflammatory medicines, such as ibuprofen, in the form of a cream or gel that you can put directly onto your skin. You can also take anti-inflammatory medicines as tablets, but wait until 48 hours after the injury before you start taking them. This is because anti-inflammatory tablets can slow down healing if you take them straight after an injury.
Some people can't use ibuprofen or other non-steroidal anti-inflammatory drugs (NSAIDs), or should only do so with caution. NSAIDs are known to cause side-effects to the digestive system and this risk is highest for elderly people. If you have asthma, you should also use NSAIDs with caution. Talk to your pharmacist or your GP about what is best for you. If your pain is severe, you may need to have a stronger anti-inflammatory medicine prescribed by your doctor, or another treatment.
Can I use a gel or spray painkiller directly on my skin instead of tablets? Are these effective?
Answer
Non-steroidal anti-inflammatory painkillers can be used in the form of a gel, cream or spray that you can use directly on your skin. This kind of painkiller may help to ease your pain in the first week after your injury. If your pain continues after this time, you may find other kinds of painkillers more effective.
Explanation
Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen can help relieve the pain and inflammation caused by a knee sprain or strain. NSAIDs such as ibuprofen and ketoprofen are available as gels, creams and sprays that you can put directly onto your skin and gently massage in, as well as tablets or capsules that you take by mouth.
You can buy some NSAIDs in gel or spray form from your pharmacist and others are available on prescription from your doctor. These kinds of painkillers do work for sprains and strains and can help to ease your pain for up to a week after an injury. As your injury starts to heal and the pain and swelling go down, painkillers that you put on your skin become less effective.
If you’re at particular risk of side-effects to your digestive system (gastrointestinal side-effects) from NSAIDs in tablet or capsule form, creams, gels or sprays may be a good alternative, but check with your pharmacist or doctor first. If you have been told you can't take NSAIDs as tablets – for instance if you’re allergic to them or have asthma – you shouldn't use creams, gels or sprays containing these medicines. Don't use these products if your skin is broken.
Can arnica help with my knee injury?
Answer
It's unlikely. There is no convincing evidence that arnica can help with sprains and strains.
Explanation
Arnica is often promoted as a treatment to help relieve soft-tissue injuries such as sprains and strains. You can buy arnica as a herbal remedy (usually as an oil) and also as a homeopathic medicine. There haven't been any studies on herbal arnica remedies. Arnica as a homeopathic remedy for sprains and strains has been studied. However, these studies didn't show any convincing evidence that arnica can help with sprains or strains.
Is a knee injury more likely because I have osteoarthritis?
Answer
Osteoarthritis can sometimes cause muscle weakness in your knee and therefore place extra strain on the ligaments.
Explanation
Osteoarthritis that affects the knee can sometimes cause damage to your ligaments and muscles. If this happens, the knee joint can sometimes ‘give way’. However, by keeping active and regularly exercising your knee, you can help to prevent this kind of injury. There is some evidence that exercise can also reduce the pain you feel from osteoarthritis of the knee and help to prevent longer term disability.
You may be asked to try a combination of different types of exercise. Strengthening exercises will help improve the muscles around your joints – this will help to stabilise your joints and also help with your pain. Also try to do some aerobic activity – anything that increases your heart rate and makes you slightly out of breath. This type of exercise can help to reduce pain, and also improve your general health and well-being. Aerobic activity can also help you to lose excess weight or control your weight, which reduces your chances of your knee problems getting worse in the future.
Range-of-movement exercises and stretches are also important to keep you flexible and mobile. This type of exercise involves moving your joints through their full range of movement and trying to move a little further beyond this.
As well as generally keeping active, your physiotherapist may also advise you to do some specific exercises for your knee. These are called quadriceps or thigh muscle exercises. Your quadriceps muscles are at the front of your thighs. They become weaker when you have osteoarthritis so exercising and strengthening them is important. By doing this, you can help to reduce your pain and stay as mobile as possible. These exercises include straight leg raises, muscle stretches and muscle clenching.
It's important to get advice about which types of exercise are best for you. This will help prevent you putting strain on individual joints and muscles that can lead to injury and longer-term problems. Your GP may refer you to a physiotherapist, specialist nurse or rheumatologist (a specialist dealing with the musculoskeletal system, the joints and surrounding tissues) for specialist advice.
Further information
Chartered Society of Physiotherapy
www.csp.org.uk
Sources
- Levy D, Dickey-White H, Sanson E. Knee injury: Soft Tissue. eMedicine. www.emedicine.medscape.com, accessed 25 February 2009
- Sprains and strains. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 25 February 2009
- Diagnosis and management of soft tissue knee injuries: internal derangements. New Zealand Guidelines Group, 2003. www.nzgg.org.nz
- MacAuley D. Oxford handbook of sport and exercise medicine. 1st ed. Oxford: Oxford University Press, 2007:205–31
- Annunziata C, Ignacio E. Patellar tendon rupture. eMedicine. www.emedicine.medscape.com, accessed 25 February 2009
- Baker B, Lubowitz J. Meniscus injuries. eMedicine. www.emedicine.medscape.com, accessed 25 February 2009
- Starting to exercise. Bandolier. www.medicine.ox.ac.uk, accessed 25 March 2009
- Herbert RD, de Noronha, M. Stretching to prevent or reduce muscle soreness after exercise. Cochrane Database of Systematic Reviews. 2007, Número 4. Art No.: CD004577. DOI: 10.1002/14651858.CD004577.pub2, www.cochrane.org
- Khan KM, Scott A. Mechanotherapy: how physical therapists’ prescription of exercise promotes tissue repair. British Journal of Sports Medicine 2009;43:247–52.
















