Type 1 Diabetes
This factsheet is for people who have type 1diabetes, or who would like information about it.
Type 1 diabetes is a lifelong condition in which the body can't control levels of glucose in the blood. It develops when the body can't produce the hormone insulin. Type 1 diabetes is sometimes called insulin-dependent diabetes.
About type 1 diabetes
Symptoms of type 1 diabetes
Complications of type 1 diabetes
Causes of type 1 diabetes
Diagnosis of type 1 diabetes
Treatment of type 1 diabetes
About type 1 diabetes
Type 1 diabetes can develop at any age, but usually affects people before the age of 40, and most commonly during childhood. It develops when your body can't produce the hormone insulin. Insulin regulates the level of glucose in your blood. Glucose is a simple form of sugar found in foods and sugary drinks. It's absorbed by your body as a natural part of digestion and is carried around your body in your blood. When glucose reaches your body tissues, such as muscle cells, it's absorbed and converted into energy.
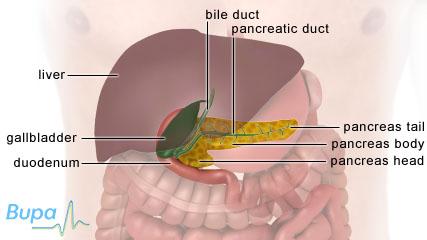
Insulin is secreted into your blood by your pancreas, which is a gland located behind your stomach. A shortage of insulin causes glucose to build up in your blood.
Symptoms of type 1 diabetes
If you have type 1 diabetes, you may:
- pass more urine than usual
- be constantly thirsty
- have unexplained weight loss
- be extremely tired
- have blurred vision
- be irritable
The symptoms can develop quickly, usually over a few weeks.
If you have any of these symptoms, see a doctor.
Complications of type 1 diabetes
If type 1 diabetes isn't diagnosed or controlled properly, you can develop blood glucose levels that are either too high (hyperglycaemia) or too low (hypoglycaemia).
Hyperglycaemia
Your blood glucose levels can become too high if you're stressed or unwell, your insulin dose is too low, you miss doses, or if you eat too much carbohydrate. Hyperglycaemia can cause you to be more thirsty than usual, feel tired and have headaches.
Rarely, glucose can build up in your blood and reach dangerous levels. This is called diabetic ketoacidosis. It can cause you to vomit, breathe faster than normal and have breath that smells of ketones (like pear drops or nail varnish). Diabetic ketoacidosis is a medical emergency and can be fatal if you aren't treated in hospital immediately.
In the long-term, hyperglycaemia can increase your risk of:
- kidney failure
- nerve damage
- blindness
- heart disease
- stroke
Hypoglycaemia
Your blood glucose levels can become too low if you don't eat enough foods that contain glucose, take too much insulin, or do more physical activity than usual. Hypoglycaemia can cause you to feel faint, sweaty, confused and you may feel your heart pounding. It should be treated straight away with glucose tablets (or a few sweets/sugary drink), followed by about two to three biscuits or a sandwich. If hypoglycaemia is left untreated you may become unconscious and if severe it can be fatal.
Causes of type 1 diabetes
Type 1 diabetes develops when the cells in your pancreas that make insulin (beta cells) are destroyed by your body's immune system. Because of this, type 1 diabetes is known as an autoimmune disease. However, the way in which type 1 diabetes first starts isn't fully understood at present, though it's possible it may be caused by a virus or run in families.
Diagnosis of type 1 diabetes
The doctor will ask about your symptoms and examine you. He or she may also ask about your medical history.
You may need to have some of the following tests.
- Urine test. You will need to give a sample to be tested for glucose and ketones.
- Fasting blood glucose test. Your doctor will arrange for you to have a sample of blood taken from your arm to test for glucose.
If your urine tests positively for ketones and you have a raised blood glucose level, this suggests a diagnosis of type 1 diabetes.
Please note that availability and use of specific tests may vary from country to country.
Treatment of type 1 diabetes
There isn't a cure for type 1 diabetes but it can be controlled with medicines and lifestyle changes and monitored with blood tests.
Medicines
Type 1 diabetes is controlled by giving your body insulin. This helps glucose to be absorbed into your cells and converted into energy, which stops it building up in your blood.
There are two main ways of taking insulin.
- Insulin injections. These are the most common form of treatment, where you inject insulin under your skin. You will usually inject yourself before meals, using either a small needle or a pen-type syringe with replaceable cartridges.
- Portable insulin pumps. These may be appropriate if you find it difficult to control your blood glucose with regular injections, despite careful monitoring. Insulin pumps can be programmed to inject you with insulin at a rate that you can control.
There are several different kinds of insulin that work at different rates and act for different lengths of time. Ask your doctor for advice on which type and method is best for you.
Availability and use of different treatments may vary from country to country. Ask your doctor for advice on your treatment options.
Self-help
By making the following lifestyle changes, you can help control your blood glucose levels.
- Eat a healthy balanced diet with regular meals, three times a day. Include carbohydrates, such as pasta or potatoes in each meal. But if you have hypoglycaemia from time to time, it's a good idea to keep some sugary food or glucose tablets with you.
- Try to do at least half an hour of moderate physical activity on at least three days a week. This will help you to stay a healthy weight and control your blood glucose levels.
- Only drink alcohol in moderation and stick within the recommended daily limits.
- If you smoke, give up. Smoking is unhealthy for everyone, but it's especially important to stop if you have diabetes because you already have an increased risk of developing circulatory problems and cardiovascular disease. Smoking makes the chance of you developing these diseases even greater.
Monitoring your blood glucose level
You can use a home test kit to monitor your blood glucose level. This involves regularly taking a pinprick of blood from the side of your fingertip and putting a drop on a testing strip. A meter will read the result automatically.
Your 'normal' blood glucose range will be specific to you but a general guide for adults is:
- before meals: 4 to 7mmol/L
- after meals: less than 9mmol/L
Your doctor will show you how to monitor your blood glucose levels and tell you how often you need to check it.
You may also need to have your levels of glycosylated haemoglobin (HbA1C) tested at least twice a year. HbA1C is a protein that is produced when you have high blood glucose levels over a long period of time. The HbA1C test is done by taking blood from a vein in your arm or sometimes a drop of blood from a fingerprick. It's used to see how well you're controlling your blood sugar levels.
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email.
How important is it to manage low blood glucose level?How will having type 1 diabetes affect my work?
Can I drive if I have type 1 diabetes?
What are the different kinds of insulin?
How important is it to manage low blood glucose level?
AnswerIt's very important to keep your blood glucose levels as stable as possible if you have type 1 diabetes. If you don’t monitor your condition regularly and your blood glucose levels get low, you may become very unwell.
Explanation
Part of the treatment for type 1 diabetes is making sure that your blood glucose levels are as near to normal as possible. Your 'normal' range will be specific to you but a general guide for adults is:
- before meals: 4 to 7mmol/L
- after meals: less than 9mmol/L
A hypo can be caused if you take too much insulin. Anyone who takes insulin as a treatment for their diabetes could have a hypo. It can also be caused if you miss a meal, don’t eat enough foods containing carbohydrate or if you take part in physical activity without eating enough to compensate for it. Another cause can be drinking too much alcohol or drinking alcohol without eating beforehand.
Most people get warning signs before a hypo, such as:
- sweating
- going pale
- feeling your heart pounding
- being confused
- feeling sick
- feeling irritable
- being shaky
How will having type 1 diabetes affect my work?
Answer
Although being diagnosed with type 1 diabetes can leave you feeling worried about work, it shouldn't stop you from having an enjoyable and fulfilling career.
Explanation
Type 1 diabetes can potentially have an impact on many areas of your life, including work. How you manage your condition and control your diabetes can influence how well you cope with work and the choices you make. Your doctor or diabetes specialist nurse can give you more information and advice about your individual circumstances.
If you have type 1 diabetes, you may have to make some adjustments to suit your life at work. For example, make sure you’re as fit and well as possible. This means having well controlled blood glucose levels and taking your insulin as planned. You may need to make changes to your meals if you work shifts, or if food isn't readily available. You will need to plan ahead to make sure you keep your blood glucose levels stable.
It’s important to remember that you’re protected at work by the Disability Discrimination Act. This protects you from being discriminated against at work because you have a disability. Your employer has to make ‘reasonable adjustments’ to allow you to do your job, for example, by giving you time off for appointments or making sure you have enough breaks to eat regularly.
There are, however, some careers that you won’t be able to pursue if you have type 1 diabetes – for example, you can't join the armed forces. Also, you won’t be allowed to hold a heavy goods vehicle (HGV) licence or be a pilot. Otherwise, there are very few jobs that you will be unable to do.
Can I drive if I have type 1 diabetes?
AnswerIf your condition is under control, you should be able to drive a car, but you won't be able to drive a HGV or passenger vehicle (such as a minibus). You will need to contact the Driver and Vehicle Licensing Agency (DVLA) to inform them about your condition. You also need to tell your car insurer about your condition.
Explanation
In the interest of road safety, you must be sure that you can safely be in control of a vehicle at all times. If you have type 1 diabetes, there is a chance that your blood glucose levels could become too low (hypoglycaemia) when you’re driving. This could endanger you and other drivers.
When you apply for a driving licence you will need to let the DVLA know that you have type 1 diabetes. The DVLA will contact your doctor for more information about how your condition is managed and whether you have any complications that might make you unsafe to drive.
You will usually be given a licence that lasts for either one, two or three years and you will have your condition assessed each time you re-apply.
You will need to be able to recognise the signs of hypoglycaemia and know how to treat it if it happens when you're driving. To help prevent hypoglycaemia:
- check your blood glucose level before you start a journey
- don't drive with a blood glucose level of less than 4mmol/litre
- don't drive for more than two hours without stopping for a snack
- keep some kind of carbohydrate, such as sweets and a sugary drink, in your car
- pull over and stop somewhere safe
- take glucose tablets or some other form of fast-acting carbohydrate immediately
- leave the driver's seat and take the keys out of the ignition to make it clear that you're no longer in charge of the car
- don't start driving again until all your symptoms have gone
What are the different kinds of insulin?
AnswerThere are three groups of insulin – human, analogue and animal. Within these groups there are different types of insulin that work at different speeds and for different lengths of time in your body.
Explanation
Human insulin is actually a synthetic (artificial) version of the insulin that is naturally made in your body. Analogue insulin is a synthetic variation of human insulin. All synthetic insulin is designed to work in the same way as natural insulin. Most people use human or analogue insulin, but some still use animal insulin because it works best for them.
There are six main types of insulin:
- Short-acting insulins. These should be injected about 15 to 30 minutes before meals and can last up to eight hours.
- Intermediate-acting insulins. These are injected once or twice a day and can last up to 18 hours.
- Rapid-acting analogues. These are injected shortly before, with or after meals. They usually start working straightaway but can last up to six hours.
- Long-acting analogues. These need to be injected once a day and can last up to 24 hours.
- Mixed insulin. This is a mix of intermediate- and short-acting insulin.
- Mixed analogue. This is a mix of intermediate-acting insulin and rapid-acting analogue.
Ask at your clinic whether they run structured education classes such as DAFNE (Dose Adjustment For Normal Eating). These are four to five day intensive courses that help you learn how to adjust your insulin dose.
Further information
Diabetes UK
0845 120 2960
www.diabetes.org.uk
Sources
- Diabetes. World Health Organization (WHO). www.who.int, published January 2011
- Guide to diabetes. Diabetes UK. www.diabetes.org.uk, accessed 25 March 2011
- Diabetes mellitus. The Merck Manuals. www.merckmanuals.com, published June 2008
- Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia. World Health Organization (WHO). www.who.int, published 2006
- Diagnosis and management of type 1 diabetes in children, young people and adults. National Institute for Health and Clinical Excellence (NICE). www.nice.org.uk, July 2004
- Simon C, Everitt H, van Dorp F. Oxford handbook of general practice. 3rd ed. Oxford: Oxford University Press, 2010: 352–53
- HbA1C test. Lab Tests Online UK. www.labtestsonline.org.uk, published 29 September 2010
- Diabetes in the UK 2010: Key statistics on diabetes. Diabetes UK. www.diabetes.org.uk, published March 2010
- What is DAFNE? DAFNE. www.dafne.uk.com, accessed 7 June 2011
- Personal communication, Dr Jonathan Katz, Consultant Endocrinologist, Barnet Hospital, 8 June 2011
This information was published by Bupa's health information team and is based on reputable sources of medical evidence. It has been peer reviewed by Bupa doctors. The content is intended for general information only and does not replace the need for personal advice from a qualified health professional.
Related topics
Benefits of exercise
Healthy eating
Sensible drinking
Smoking - ways to stop
Type 2 diabetes
















