Achilles tendinopathy
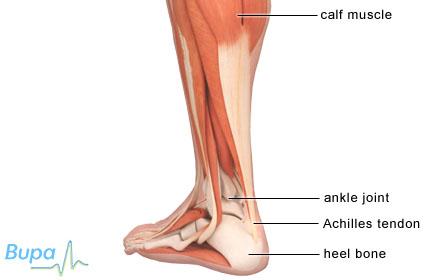
A tendon is a tissue that connects a muscle to bone. Achilles tendinopathy is when your Achilles tendon becomes injured, causing pain and stiffness just above your heel bone.
About Achilles tendinopathy
The Achilles tendon is very strong. It’s located at the back of your ankle and connects your two calf muscles to the bone in the heel of your foot. The tendon is made up of many collagen fibres.
There are several ways in which the tendon can become injured, leading to Achilles tendinopathy. The tissue surrounding the tendon may become inflamed, the tendon may become worn down (degenerate), cysts (small sacs of fluid) may form inside the tendon, or tiny tears may form in the fibres.
This type of injury occurs most often in athletes, but it can affect anyone.
Symptoms of Achilles tendinopathy
The main symptom is pain and stiffness just above your heel bone that develops gradually. At first you may only have pain after rest, such as first thing in the morning. The pain may improve with exercise to begin with.
Over time, as the problem worsens, you may have pain after exercise and finally pain during exercise. The tendon above your heel may appear slightly swollen and feel stiff.
Causes of Achilles tendinopathy
Achilles tendinopathy is usually caused by overuse and is a common injury in sports that involve running and jumping. Repeated stress on the tendon can cause microscopic changes to occur.
Achilles tendinopathy is more likely to happen if you:
- increase your activity levels too quickly (mileage, speed and type of activity)
- don’t leave enough recovery time between training sessions
- change your usual training surface
- wear inappropriate footwear
- have poor movement (biomechanics) in your feet – for example, flat feet
- have poor movement (biomechanics) in your lower limb – for example, poor calf flexibility
- have a poor range of movement in your ankle
Diagnosis of Achilles tendinopathy
Your GP or physiotherapist will ask you about your symptoms and examine you. He or she will also ask you about your medical history.
You may need to have further tests to look at the damaged Achilles tendon. These can include:
- an ultrasound scan, which uses high-frequency sound waves to produce an image of the Achilles tendon to look for any changes to the tendon tissue
- an MRI (magnetic resonance imaging) scan, which uses magnets and radiowaves to produce two- and three-dimensional pictures of the leg that can help your doctor to see if there is any fluid or tears in the Achilles tendon
Treatment of Achilles tendinopathy
Treatment depends on how serious the injury is. Achilles tendinopathy normally requires treatment.
· Self-help
There are a number of things you can do to help Achilles tendinopathy including the following:
- Wear a small heel raise in each shoe to help reduce the load on your Achilles tendon and give immediate relief of pain when walking.
- Reduce the intensity and length of time you spend exercising.
- Wear supportive footwear.
- Avoid bare feet around the house.
- Stretch your calf muscles.
- Apply ice for 10 minutes every two to three hours in the acute phase. Never apply ice directly to your skin as it can give you an ‘ice burn’ – always place a cloth between the ice and skin.
· Medicines
You can buy painkillers such as paracetamol to treat mild and moderate pain. Anti-inflammatory medicines, known as non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen also help to relieve pain and stiffness. Always read the patient information that comes with your medicine, and if you have questions, ask your pharmacist or doctor for advice.
Your doctor or physiotherapist may suggest an injection if other treatments don’t work. This is either an injection of steroid and local anaesthetic, which is directed using ultrasound, or an injection of Aprotinin. Injection therapy using Aprotinin is relatively new, so not all doctors or physiotherapists will offer it.
-
Physiotherapy
Your GP may refer you to a physiotherapist (a health professional who specialises in movement and mobility). You can also choose to see a physiotherapist privately. He or she will give you a programme that will include stretching, strengthening and icing your Achilles tendon. You should carry out the programme daily and it can take around three months before your symptoms improve. Your physiotherapist may also use various techniques to help speed up the healing of your Achilles tendon such as soft tissue massage and acupuncture.
Treatment may involve you using orthotics (special insoles you wear in your shoes) to re-align your foot and reduce stress on your Achilles tendon. This will help to alleviate your symptoms and prevent further injury.
-
Surgery
Your doctor may recommend surgery if your symptoms don’t improve after six months of treatment.
Prevention of Achilles tendinopathy
There are some precautions you can take to try to reduce the risk of damaging your Achilles tendon.
- Exercise regularly to maintain a good level of fitness. This will mean your muscles are stronger and better able to support your joints, including your knees. If you haven’t been active for a while, start gently and gradually increase the intensity and length of time you spend exercising.
- Spend five to 10 minutes warming up before exercise to increase blood flow to your muscles and reduce the chance of an injury. Many sports professionals advise stretching your muscles after warming up and again after cooling down; however the benefit of stretching before or after exercise is unproven. You can include a calf muscle stretch, which will lengthen the Achilles tendon.
If performing high-impact exercise such as running, take your running shoes to a specialist shop and ask for advice about whether they are right for running. An experienced adviser will watch you run and can recommend suitable shoes for you.
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email.
I have Achilles tendinopathy. How long will it take to heal?
Answer
This will depend on the severity of your injury. The key to successful recovery of Achilles tendinopathy is early diagnosis, and correcting the factors that have caused the injury, such as muscles tightness. It’s also important that you follow a strengthening programme and return to physical activity gradually.
Explanation
If you have Achilles tendinopathy mildly, it's likely to take around three months to heal. If your injury is more severe, full recovery can take up to six months. It’s important that you start your treatment early and make sure that you follow a strengthening programme.
There are a number of things you can do to help Achilles tendinopathy including the following:
- Wear a small heel raise in each shoe to help reduce the load on your Achilles tendon and give immediate relief of pain when walking.
- Reduce the intensity and length of time you spend exercising.
- Wear supportive footwear.
- Avoid bare feet around the house.
- Stretch your calf muscles.
- Apply ice for 10 minutes every two to three hours in the acute phase. Never apply ice directly to your skin as it can give you an ‘ice burn’ – always place a cloth between the ice and skin.
When can I return to activity after treatment for Achilles tendinopathy?
Answer
It’s important that you return to physical activity gradually. A good indicator is when there is no longer pain or stiffness in the Achilles tendon first thing in the morning.
Explanation
You can begin physical activity when your symptoms have improved and the tenderness has settled. You may need to wear a heel raise in your shoes to reduce the stress on your Achilles tendon.
Start by jogging and gradually increase the time until you can jog comfortably for 30 to 45 minutes. You shouldn’t feel any pain during or after exercise. You can then begin to increase your speed and finally introduce sprint work and hill running. It’s important that you don’t push yourself.
Most people with Achilles tendinopathy get better and don’t have any long-term problems. If you’ve had surgery, the Achilles tendon may remain weak in the first six to nine months. This can have an impact on your return to sport.
What type of shoe should I wear to help relieve pain in my Achilles tendon?
Answer
Your physiotherapist may recommend that you wear a heel raise in both shoes to reduce the load on your Achilles tendon. You will be able to stop wearing the heel raise once your calf is lengthened.
Explanation
Orthotics are special insoles worn in your shoe that aim to realign your foot and correct poor biomechanics. You can buy ready made orthotics or have them custom made. It’s important to seek the advice of a professional, such as a podiatrist, before using orthotics as the wrong type of device may do more harm than good.
If you’re concerned about whether your shoes are right for running, it's a good idea to take them along to a specialist running shop and ask for advice. A general sports shop won't be able to offer you the advice you need. You will also need an experienced adviser to watch you run and recommend suitable shoes for you. You will probably be asked to run on a treadmill in the shop, or you may be asked to run up the street outside as the advisor watches your feet. Once they have identified whether you’re a neutral runner or if you overpronate or underpronate, and what you will be using the shoes for, the advisor can recommend a couple of pairs of trainers from a range of brands.
When not exercising, try to wear supportive shoes with good cushioning in the soles and avoid walking barefoot around the house.
Wearing high heels shortens the calf muscle and Achilles tendon. Tight calf muscles can increase your risk of developing Achilles tendon injuries. It’s important that you don’t wear high heels to prevent Achilles tendinopathy.
Further information
British Orthopaedic Foot and Ankle Society
www.bofas.org.uk
Sources
- Achilles tendon. British Orthopaedic Foot and Ankle Society. www.bofas.org.uk, accessed 9 July 2009
- Maffulli N, Sharma P, Luscombe KL. Achilles tendinopathy: aetiology and management. J R Soc Med 2004; 97:472–76. www.jrsm.rsmjournals.com
- MacAuley D. Oxford handbook of sport and exercise medicine. 1st ed. Oxford: Oxford University Press, 2007:272
- Kader D, Saxena A, Movin T, et al. Achilles tendinopathy: some aspects of basic science and clinical management. Br J Sports Med 2002; 36:239–49. www.bjsm.bmj.com
- Brukner P, Khan K. Clinical sports medicine. 2nd ed: McGraw Hill, 2005:540–42
This information was published by Bupa’s health information team and is based on reputable sources of medical evidence. It has been peer reviewed by Bupa doctors. The content is intended for general information only and does not replace the need for personal advice from a qualified health professional.














