Achilles tendon rupture
A tendon is a tissue that connects a muscle to bone. An Achilles tendon rupture is when the Achilles tendon in the lower leg is torn, either partially or completely. It’s the most frequently ruptured tendon in the body.
About Achilles tendon rupture
Symptoms of Achilles tendon rupture
Causes of Achilles tendon rupture
Diagnosis of Achilles tendon rupture
Treatment of Achilles tendon rupture
Prevention of Achilles tendon rupture
About Achilles tendon rupture
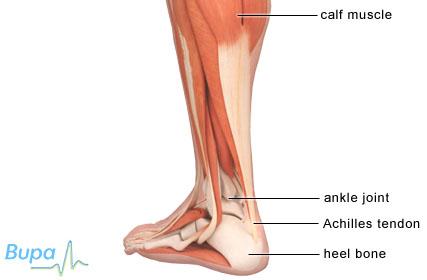
The Achilles tendon is very strong and flexible. It's found at the back of your ankle and connects your calf muscle to the bone in the heel of your foot (calcaneum). When an Achilles tendon rupture happens you may partially or completely tear the tendon.
This type of injury occurs most often in athletes or people between the age of 30 and 50, but it can affect anyone. Complete rupture is more common in men.
Symptoms of Achilles tendon rupture
If you rupture your Achilles tendon you will feel a sharp pain in the back of your leg and you will be unable to flex your ankle or point your toes. You may:
- have swelling in your lower leg
- be unable to put your full weight on your ankle
- hear a snapping or tearing sound when it happens
- have a limp, and be unable to stand on tiptoe or climb stairs
- develop bruising
When the injury occurs, you may feel like you have been kicked or hit in the back of the leg.
Causes of Achilles tendon rupture
Achilles tendon rupture is most likely to happen when your leg is straight and your calf muscle is contracted during activities such as running, jumping or playing sport such as football or tennis.
There is a very small risk of Achilles tendon rupture if you have Achilles tendinopathy. Achilles tendinopathy is pain, thickening and stiffness in your Achilles tendon both during exercise and often following exercise.
Certain medicines taken together may increase the risk of Achilles tendon injuries. These are quinolone antibiotics (eg ciprofloxacin) and corticosteroids. The exact risk of Achilles tendon rupture caused by these medicines isn't clear.
Diagnosis of Achilles tendon rupture
Si usted sufre una rotura de dicho tendón, debe dirigirse de inmediato a un departamento de If you have a rupture, you must go straight to an accident and emergency department or to your GP. The doctor you see will ask about your symptoms and examine you. You will be referred to a specialist for treatment. Your doctor may ask you to do a series of movements or exercises to see how well you can move and how affected your lower leg is. These may include squeezing your calf muscle or asking you to try to stand on tiptoe.
At the hospital, you may have further tests to look at your Achilles tendon. These may include:
- an ultrasound scan, which uses sound waves to produce an image of the inside of a part of the body
- an MRI (magnetic resonance imaging) scan, uses magnets and radiowaves to produce images of the inside of the body
Treatment of Achilles tendon rupture
Achilles tendon ruptures are treated using surgery, or by keeping it immobile while it heals. The treatment you have may depend on how much time has passed since the injury, your age and how active you are.
Whether you have an operation or not, you will have a plaster cast on your lower leg and won’t be able to put weight on it for at least four weeks.
You can take painkillers that you would usually take for a headache, for example a non-steroidal anti-inflammatory painkiller such as ibuprofen. Always read the patient information leaflet that comes with your medicine.
Surgery
Surgery is usually recommended for active young people.
There are two types of surgery used to repair a ruptured Achilles tendon:
- open surgery, which is when one long cut is made to reach the tendon to repair it
- percutaneous surgery, which is when a number of small cuts are made to reach the tendon to repair it
Both types of surgery involve stitching the tendon together so it can heal. Open surgery is less likely to cause injury to one of the nerves in your leg.
After surgery you will have a series of casts or an adjustable brace on your leg to help the Achilles tendon heal. This will usually be for between four and eight weeks.
About five in 100 people who have surgery for this injury get an infection. This can be treated with antibiotics. There may be a lower risk of infection if you have percutaneous surgery. For between one and three in 100 people the tendon will re-rupture after the operation.
Non-surgical treatment
A cast or brace is put onto your lower leg to help the tendon heal. You will have to wear a cast or brace for at least six to eight weeks. During this time the cast will be changed a number of times to make sure the tendon heals in the right way. It usually takes longer to recover from Achilles tendon rupture using this treatment, compared with surgery.
There is no risk of infection from this type of treatment and it's suitable for people who may have complications during surgery.
The tendon may re-rupture in about 13 in every 100 people who have this treatment.
If your tendon is partially ruptured you’re more likely to be given a cast or brace, instead of surgery.
After your treatment
Once your cast or brace is removed you will need to gradually increase your activity to strengthen the tendon. Your doctor, or a physiotherapist, will give you a number of exercises to do, which will increase the range of movement and strength in your lower leg. Your physiotherapist may try various techniques to reduce the pain. These may include exercises and soft tissue techniques (deep tissue massage). He or she will also advise you on returning to exercise. You should be able to return to your usual level of activity six months after your injury. However, this may take longer and will also depend on the activity.
Prevention of Achilles tendon rupture
There are ways to reduce the risk of injury to your Achilles tendon. To prevent injury when starting a new exercise regime, gradually increase the intensity and the length of time you spend being active.
Warming up your muscles before you exercise and cooling them down after you have finished may help. Five to 10 minutes of low intensity activity, such as brisk walking, is enough for a warm up and this is also needed for a cool down. You can do a series of muscle stretches to help prevent injuries after your warm up and cool down. This can include a calf muscle stretch, which will lengthen the Achilles tendon before you exercise.
Answers to questions about Achilles tendon rupture
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email. This section will expand over time.
Will achilles tendon rupture get better on its own, without treatment?
Will I be able to walk once my achilles tendon rupture is treated?
Will I have to give up running or sport after Achilles tendon rupture?
Will achilles tendon rupture get better on its own, without treatment?
No, it won’t get better on its own. You will need medical treatment.
Explanation
A ruptured Achilles tendon won’t heal on its own without treatment.
If your tendon ruptures then the sooner you seek treatment, the more choice of treatment you will have and the better your chances of a full recovery. If you need to have surgery, it should be done as soon after the injury as possible. A delay in having surgery can cause the two ends of the Achilles tendon to separate and shorten, which makes reattaching the two ends difficult.
Will I be able to walk once my achilles tendon rupture is treated?
For about four to six weeks after your injury you won’t be able to walk on your affected leg, or put any weight on it. You will be able to walk without putting weight on your affected leg using crutches. After this you can gradually start to walk again.
Explanation
Initially you won’t be able to put weight, or walk, on your affected leg. This is usually for between four and six weeks after treatment.
After this period you should be able to gradually put weight on your affected leg – doctors call this weight-bearing. You may need to wear a shoe with a one inch heel or a shoe insert for a number of weeks after this. This helps to place the tendon in the best position to heal. Your doctor or physiotherapist will advise when you can begin to put weight on your affected leg.
Will I have to give up running or sport after Achilles tendon rupture?
Most people recover fully and are able to return to running or sport after an Achilles tendon rupture.
Explanation
How well you recover after the rupture of your Achilles tendon will depend on your age, the kind of treatment, your rehabilitation after treatment, the amount of rehabilitation exercises you do, and the level of activity you’re aiming to get back to.
Following treatment and rehabilitation most people are able to return to the level of activity they had before the injury. This includes athletes. However, if you have a cast or brace rather than surgery to repair the injury then the tendon is more likely to rupture again. Some people who have surgery may not be able to recover enough strength and flexibility in the tendon to go back to sport or running.
You should stretch and warm up and cool down well before and after you exercise. It’s important to wear well fitting shoes that are right for the activity you’re doing. This can help to prevent the Achilles tendon from rupturing again.
Further information
British Orthopaedic Foot and Ankle Society (Sociedad Británica de Ortopedia del Pie y el Tobillo)
www.bofas.org.uk
Sources
- Achilles tendon rupture. eMedicine. www.emedicine.medscape.com, consultado el 23 de febrero de 2010
- MacAuley D. Oxford Handbook of Sport and Exercise Medicine. 1st ed. 2007 Oxford: Oxford University Press. p 272
- Achilles tendinopathy. Clinical Knowledge Summaries. www.cks.nhs.uk, consultado el 23 de febrero de 2010
- Quinolones and Achilles tendon rupture. Bandolier. www.medicine.ox.ac.uk, consultado el 23 de febrero de 2010
- Ruptured Achilles tendons. Bandolier. www.medicine.ox.ac.uk, consultado el 25 de febrero de 2010
- Starting to exercise. Bandolier. www.medicine.ox.ac.uk, consultado el 25 de febrero de 2010.















