Alcohol dependence

Alcohol dependency is an overpowering urge to drink. It’s most common in people with anxiety, depression or who have a lot of stress in their job.
About alcohol dependence
Symptoms of alcohol dependence
Complications of alcohol dependence
Causes of alcohol dependence
Diagnosis of alcohol dependence
Treatment of alcohol dependence
Preventing a relapse
About alcohol dependence
Alcohol is an addictive drug and you can become psychologically and physically dependent on it. In the UK, around nine in 100 men and four in 100 women are dependent on alcohol.
Alcohol dependence – or ‘alcohol dependence syndrome’ (formerly known as alcoholism) is a pattern of routinely drinking excessive amounts of alcohol over a long period of time, which results in addiction. It can be associated with psychological and physical health problems and can seriously affect your relationships with family and friends. It can also affect your job.
Symptoms of alcohol dependence
Alcohol dependence is usually characterised by an overpowering urge to drink alcohol and the inability to limit or stop drinking once you have started. Some people who are dependent on alcohol report being preoccupied with it and that the need to drink alcohol takes over their lives.
If you drink regularly, your body gets used to lots of alcohol and you may find that you need to drink increasingly more to feel its effects. This is known as alcohol tolerance and has a role in a person becoming addicted to alcohol.
Other symptoms of alcohol dependence include:
- neglecting other interests in favour of pursuits that involve alcohol
- spending more time drinking and recovering from the effects of alcohol than you used to
- drinking before midday
- anxiety or irritability
- feeling that you can’t cut down on your drinking despite signs that it’s damaging your psychological or physical health, your personal relationships or your work
Another sign that you’re dependent on alcohol is if you suffer from physical withdrawal symptoms when you stop drinking. You may feel the need to drink to avoid or relieve such symptoms. Withdrawal symptoms include:
- shaking or tremors
- feeling or being sick first thing in the morning
- sweating a lot
- finding it difficult to sleep
- feeling your heart race
- anxiety or irritability
Complications of alcohol dependence
If you drink large amounts of alcohol, you are at greater risk of having:
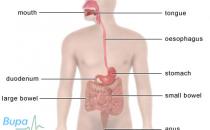
- liver disease (such as fatty liver, alcoholic hepatitis or alcoholic cirrhosis)
- high blood pressure and other heart problems (such as heart muscle damage, heart disease and stroke)
- cancer (such as cancer of the liver, stomach, bowel, rectum, lung, pancreas and breast)
- memory loss
- depression
- suicidal feelings
- problems with your sex life
- alcoholic dementia
- pancreatitis
Another potential complication is delirium tremens which may occur with acute alcohol withdrawal. This causes symptoms such as shaking, sweating, diarrhoea and seizures. It may also cause anxiety, confusion, paranoia and hallucinations (where you see and/or hear things that aren’t there). Delirium tremens requires urgent medical attention as it can be life threatening.
Causes of alcohol dependence
People drink alcohol for many different reasons. Many people who become dependent on alcohol use it as a way of dealing with anxiety and depression.
Although it may help you dismiss your problems in the short term, alcohol actually makes anxiety and depression worse. It does this by interacting with chemicals called neurotransmitters in your brain which naturally help you fight depression and anxiety.
Social factors, such as the affordability and availability of alcohol, peer pressure and the buying of rounds in groups are also thought to have a role in causing alcohol dependency.
Diagnosis of alcohol dependence
Acknowledging that alcohol is having a negative impact on your life is an important first step in your diagnosis and successful treatment.
If you feel that you may be alcohol dependent, see your GP. He or she will ask about your symptoms and may examine you.
Your GP will ask about your drinking, how you feel about it and its effect on your life and wellbeing. He or she may ask you the following four questions to establish if you are alcohol dependent. These are known as the CAGE questions.
- Have you ever felt you should Cut down on your drinking?
- Have people Annoyed you by criticising your drinking?
- Have you ever felt bad or Guilty about your drinking?
- Have you ever had a drink first thing in the morning to steady your nerves or to get rid of a hangover (Eye opener)?
If your lifestyle, psychological or physical illness or the score on the CAGE indicates you may be drinking too much, your GP may refer you to specialist alcohol services. In most areas in the UK, you can self-refer to alcohol services. Your GP may ask you to do this because it’s an important step for you to be active and take control of your own addiction.
Treatment of alcohol dependence
Your treatment will be tailored to suit you and will depend on how much you drink, and any associated physical or mental health problems that you may have.
Your GP will assess your level of alcohol dependence. If you have severe alcohol dependence, especially if there is evidence of physical damage to your internal organs such as your liver, then your doctor is likely to advise you to cut down on alcohol with the aim of stopping drinking completely. This is called abstinence.
However, it’s recognised that some people have a lower level of alcohol dependence and may not be willing to give up alcohol completely. It’s important to work with your doctor to agree on a treatment plan that is realistic for you, and which you can stick to, and in this case it may be that you aim to cut down your drinking to a controlled, lower level.
There are many professional services and groups that can give you the help and support you need to stop drinking.
Self-help
Acknowledging that you’re dependent on alcohol and finding the determination to change and the will-power to do so is important for successful treatment. There are a number of self-help tools such as information leaflets and websites that can help you to stop drinking.
Detoxification
If you’re a heavy drinker, you may need to be supervised by health professionals while you give up. This is because the physical withdrawal symptoms associated with stopping drinking can carry risks. Detoxification or “detox” is a planned withdrawal from drinking alcohol and may involve taking a short course of medicine to help prevent withdrawal symptoms.
Benzodiazepine medicines, such as diazepam or chlordiazepoxide hydrochloride, are most commonly used during detoxification. Your GP may prescribe these for you to take at home or you may need to stay in a specialist treatment centre during detoxification. Medicines are only available as a short-term treatment to help you gain control and not a long-term solution.
Counselling
Many people find that talking to someone about their problem is a useful and important part of treatment. You may wish to speak to your GP or trained counsellors who can help you understand the reasons for your drinking, and give you skills to control or stop the urge to drink.
Your partner or family may also be invited to attend counselling with you and be involved in your treatment.
Mutual-help support groups
There are many people in the UK who are dependent on alcohol and who support each other by sharing personal experiences and advice. Mutual-help support groups can help you while you’re giving up and can also help prevent you becoming dependent again. Support groups such as Alcoholics Anonymous and Al-Anon (a support group for family and friends of those who are alcohol dependent) can be found nationwide.
Dietary supplements
Some people who are alcohol dependent are deficient in vitamins and minerals; vitamin B1 (thiamine) deficiency is the most common. Your doctor may prescribe thiamine tablets and also ask you to take multivitamins.
Alcohol and pregnancy
Drinking alcohol during pregnancy can affect the development of your unborn baby and may cause your baby to have a condition called fetal alcohol syndrome. Drinking during pregnancy can also increase the chance of having a miscarriage.
Preventing a relapse
After you have successfully given up drinking, starting again (or relapsing) is common. There are a number of ways that you can plan ahead and minimise the risks of this happening to you. It’s important to remember that treatment for alcohol dependence is an ongoing process. You’re more likely to successfully give up drinking if you receive help and support from family and friends, mutual-help support groups, your GP or from a counsellor.
There are medicines that your doctor may prescribe which can help prevent your cravings for alcohol (such as acamprosate calcium) or other medicines (such as disulfiram), which help deter you from drinking by giving you unpleasant symptoms such as vomiting and a headache if you drink alcohol.
How many units does someone need to drink to be classed as alcohol dependent?
I’m worried that my partner has a drink problem but denies it? What should I do? How do I make them see they have a problem and get help
Why are people who are alcohol dependent sometimes undernourished? I thought that alcohol was high in calories?
Does alcohol dependence run in families
How am I likely to feel when I give up drinking?
Should I set a date and stop drinking completely on that day or should I cut down gradually over a period of time?
I drink to help me cope with my feelings but what else could I do to improve the way I think and feel?
I have given up drinking alcohol and am finding it difficult to get to sleep. Is there anything can try?
How many units does someone need to drink to be classed as alcohol dependent?
Alcohol dependence isn’t diagnosed by how many units of alcohol you drink, but your dependence on or addiction to what you drink, however much that may be.
Explanation
Alcohol dependence isn’t related to the amount you drink in any given period; it’s rather the pattern of dependence or addiction to what you drink. However, if you drink regularly, your body gets used to lots of alcohol and you may find that you need to drink increasingly more to feel the effects. This is known as dependency and plays a key part in you becoming addicted to alcohol. If you drink to deal with ongoing or underlying problems, such as stress, you’re also at greater risk of becoming dependent.
Further information
Alcohol Concern
020 7264 0510
www.alcoholconcern.org.uk
Sources
- Cheers? Understanding the relationship between alcohol and mental health. Mental Health Foundation, 2006. www.mentalhealth.org.uk
- Alcohol problem drinking. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 4 February 2010
- Alcohol use disorders: Physical complications. National Institute for Health and Clinical Excellence (NICE), 2009. www.nice.org.uk
- Ferri M, Amato L, Davoli M. Alcoholics anonymous and other 12-step programmes for alcohol dependence. Cochrane Database of Systematic Reviews 2006, Issue 3. www.cochrane.org
I’m worried that my partner has a drink problem but he denies it. What should I do? How do I make him see he has a problem and get help?
If you’re worried that somebody close to you is drinking too much or is dependent on alcohol, contact a support group, your GP or a counsellor and speak to them for advice.
Explanation
You can’t force someone to seek help, it can lead to conflict and have a negative impact on their drinking. It is the person themselves who needs to understand and has to do something about their problem. Support groups for friends and relatives of people who are alcohol-dependent (such as Al-anon), can help understand the ways that you can help your loved one come to the conclusion that they need to seek help for themselves and become active in the process.
Further information
Al-Anon
020 7403 0888
www.al-anonuk.org.uk
Source
What is al-anon? Al-Anon. www.al-anonuk.org.uk, accessed 8 February 2010
Why are people who are alcohol dependent sometimes undernourished? I thought that alcohol was high in calories?
Alcohol is high in calories but doesn’t contain any vitamins. Also, some heavy drinkers neglect eating a healthy balanced diet.
Explanation
Alcoholic drinks are high in calories and are known as ‘empty calories’ because they have no nutritional value. This is why if you drink a lot you may put on weight but be undernourished. Also, if you drink heavily, you may neglect your diet and fail to eat a balanced diet rich in vitamins and minerals. Further to this, alcohol also reduces your body’s ability to absorb vitamins from the food that you eat.
Most commonly, people who are alcohol dependent are deficient in vitamin B1 (thiamine). Your doctor can prescribe thiamine tablets. Vitamin B1 deficiency is linked to brain and nerve damage and if you’re in hospital it may be given to you as an injection to ensure that it reaches your brain quickly.
Further information
Alcohol Concern
020 7264 0510
www.alcoholconcern.org.uk
Sources
- Alcohol - problem drinking. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 4 February 2010
- Long-term effects of alcohol on the body. Infoscotland. www.infoscotland.com, accessed 8 February 2010
- Vitamin B group. British National Formulary. www.bnf.org, accessed 14 February 2010
Does alcohol dependence run in families?
Yes, alcohol dependency may run in some families, but it’s thought there are a range of factors involved in becoming dependent on alcohol.
Explanation
There is some evidence to suggest that genetic influences (family history) may play a role, not only in whether you like the taste and effect of drinking alcohol, but whether or not you have a tendency to become addicted or dependent on it. However, social, personal and work factors can also play a role in alcohol dependence and because someone in your family has a drink problem, it doesn’t mean that you will have one too.
Further information
Alcohol Concern
020 7264 0510
www.alcoholconcern.org.uk
Sources
- Alcohol - problem drinking. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 4 February 2010
- Ferri M, Amato L, Davoli M. Alcoholics anonymous and other 12-step programmes for alcohol dependence. Cochrane Database of Systematic Reviews 2006, Issue 3. www.cochrane.org
How am I likely to feel when I give up drinking?
People differ in how they feel when they stop drinking; some find it easy while others find it very difficult. There are some withdrawal symptoms that you may experience.
Explanation
In the first few days after you stop drinking you may experience some withdrawal symptoms. For a few days you may:
- have shakes or tremors
- feel or be sick
- sweat a lot
- find it difficult to sleep
- feel your heart beating rapidly
- feel anxious
It’s important to remember that the first few days are the worst and that the symptoms will wear off.
Your doctor may prescribe medicines that can help your body adjust to the absence of alcohol and reduce withdrawal symptoms. If you’re a heavy drinker, withdrawal symptoms associated with stopping drinking can carry risks. These include delirium tremens, which requires urgent medical attention. So, you may need medical supervision in a rehabilitation centre for example, while you give up.
Further information
Alcohol Concern
020 7264 0510
www.alcoholconcern.org.uk
Sources
- Alcohol - problem drinking. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 4 February 2010
- Alcohol use disorders: Physical complications. National Institute for Health and Clinical Excellence (NICE), 2009. www.nice.org.uk
- Ferri M, Amato L, Davoli M. Alcoholics anonymous and other 12-step programmes for alcohol dependence. Cochrane Database of Systematic Reviews 2006, Issue 3. www.cochrane.org
Should I set a date and stop drinking completely on that day or should I cut down gradually over a period of time?
Both approaches are used by people wanting to cut down or stop drinking alcohol. Speak to your GP about which method would be most suitable for you.
Explanation
If you cut down your alcohol consumption over a period of seven days, this may reduce any mild withdrawal symptoms. Some people find this hard to do and setting a date on which to give up is a more successful approach.
Discuss with your GP which way of giving up would best suit you. You may be advised to be in contact with a medical professional when you stop drinking in case of adverse withdrawal symptoms (such as delirium tremens, which requires urgent medical attention). Your GP may also prescribe medicines that will help your body to adjust and reduce withdrawal symptoms when you stop drinking.
Further information
Alcohol Concern
020 7264 0510
www.alcoholconcern.org.uk
Sources
- Alcohol - problem drinking. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 4 February 2010
- Alcohol use disorders: Physical complications. National Institute for Health and Clinical Excellence (NICE), 2009. www.nice.org.uk
- Alcohol dependence. British National Formulary. www.bnf.org, accessed 14 February 2010
I drink to help me cope with my feelings but what else could I do to improve the way I think and feel?
There are many ways that you can improve the way you think and feel other than through drinking. If you think you’re experiencing psychological problems, see your GP.
Explanation
There are a number of ways you can help yourself feel better. Why not try some of the following to improve your wellbeing.
- Take regular exercise – there is evidence that exercise is linked to good mental health.
- Eat a balanced diet rich in vitamins.
- Ask for help when you need it.
- Share your problems and feelings with others, either family or friends or with a trained counsellor.
- Take a break from your regular routine from time to time.
Further information
Mental Health Foundation
www.mentalhealth.org.uk
Sources
- Cheers? Understanding the relationship between alcohol and mental health. Mental Health Foundation, 2006. www.mentalhealth.org.uk
- Alcohol - problem drinking. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 4 February 2010
- Physical activity. Department of Health. www.dh.gov.uk, accessed 8 February 2010
- Mead Ge, Morley W, Campbell P, et al. Exercise for depression. Cochrane Database of Systematic Reviews 2009, Issue 3. www.cochrane.org
I have given up drinking alcohol and am finding it difficult to get to sleep. Is there anything I can try?
Yes, there is a range of self-help methods you can try to help you get to sleep.
Explanation
Some of the following techniques may help you drift off.
- Take more physical exercise.
- Don’t drink anything that contains caffeine (such as tea and coffee) in the evening.
- Have a healthy snack or drink before bedtime, such as hot milk and toast with honey.
- Relax before you go to bed – for example listen to some gentle music as you lie in bed with your eyes closed, relax your body. This will help you rest even if you don’t sleep.
- If you find yourself lying there worrying, write your worries down and then imagine them floating away to be dealt with in the morning.
If you find you are still having difficulties with sleeping after trying these measures, ask your doctor for advice.
Further information
-
Mental Health Foundation
www.mentalhealth.org.uk
Sources
·Sleeping well. Royal College of Psychiatrists. www.rcpsych.ac.uk, accessed 8 February 2010
·Insomnia. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 8 February 2010
- Cheers? Understanding the relationship between alcohol and mental health. Mental Health Foundation, 2006. www.mentalhealth.org.uk
- Alcohol - problem drinking. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 4 February 2010
- Statistics on alcohol, England 2009. National Statistics. www.statistics.gov.uk, accessed 4 February 2010
- Hesse M, Vanderplasschen W, Rapp RC, et al. Case management for persons with substance use disorders.
- Cochrane Database of Systematic Reviews 2007, Issue 4. www.cochrane.org
- Alcohol use disorders: Physical complications. National Institute for Health and Clinical Excellence (NICE), 2009. www.nice.org.uk
- Ferri M, Amato L, Davoli M. Alcoholics anonymous and other 12-step programmes for alcohol dependence. Cochrane Database of Systematic Reviews 2006, Issue 3. www.cochrane.org
- The management of harmful drinking and alcohol dependence in primary care. Scottish Intercollegiate Guidelines Network (SIGN), 2004. www.sign.ac.uk
- National stroke strategy. Department of Health, 2007. www.dh.gov.uk
- Alcohol: Our favourite drug. Royal College of Psychiatrists. www.rcpsych.ac.uk, accessed 8 February 2010
- Public health draft guidance: Alcohol-use disorders: Preventing the development of hazardous and harmful drinking. National Institute for Health and Clinical Excellence (NICE), 2009. www.nice.org.uk
- Gillman MA, Lichtigfeld F, Young T. Psychotropic analgesic nitrous oxide for alcoholic withdrawal states. Cochrane Database of Systematic Reviews 2007, Issue 2. www.cochrane.org
- Antenatal care. National Institute for Health and Clinical Excellence (NICE), 2008. www.nice.org.uk
- Alcohol dependence. British National Formulary. www.bnf.org, accessed 14 February 2010
- Long-term effects of alcohol on the body. Infoscotland. www.infoscotland.com, accessed 8 February 2010
- Vitamin B group. British National Formulary. www.bnf.org, accessed 14 February 2010
- Physical activity. Department of Health. www.dh.gov.uk, accessed 8 February 2010
- Mead Ge, Morley W, Campbell P, et al. Exercise for depression. Cochrane Database of Systematic Reviews 2009, Issue 3. www.cochrane.org
- Sleeping well. Royal College of Psychiatrists. www.rcpsych.ac.uk, accessed 8 February 2010
- Insomnia. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 8 February 2010
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The alcohol use disorders identification test. The World Health Organization (WHO), 2001. http://www.who.int/en/