Bowel cancer
Published by Bupa's health information team, January 2010.
This factsheet is for people who have bowel cancer, or who would like information about it.
Bowel cancer is a lump created by an abnormal and uncontrolled growth of cells in the lining of the bowel.
How cancer develops
About bowel cancer
Symptoms of bowel cancer
Causes of bowel cancer
Diagnosis of bowel cancer
Treatment of bowel cancer
Prevention of bowel cancer
How cancer develops
The information on the video provided does not constitute advice on diagnosis or the treatment for heart disease and such advice should always be sought from a doctor or another suitably qualified health professional.
About bowel cancer
Bowel cancer is the third most common cancer in the UK; around 37,000 people are diagnosed each year. It can occur at any age but is most common in people over the age of 60.
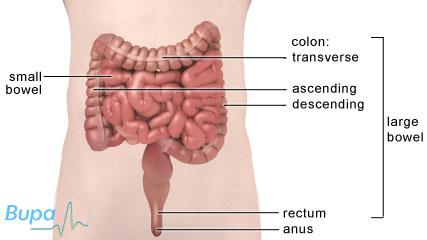
Bowel cancer, also known as colorectal cancer, is the name for any cancer of your large bowel and rectum (back passage). Very rarely, cancers can occur in your small bowel.
Your large bowel (also called your colon) is the last section of your digestive system. Food passes through your small bowel (the longer, thinner part of your bowel) where nutrients are absorbed. Food waste then travels through your large bowel, where it becomes more solid faeces.
Your large bowel has three sections: the ascending; transverse; and descending colon. Your rectum, at the end of your large bowel, is where faeces collects before passing through your anus as a bowel movement.
Usually, large bowel cancers develop from small, non-cancerous (benign) growths of tissue called polyps that can extend from the lining of your bowel wall. Sometimes polyps can become cancerous (malignant) over time. If the cancer isn’t treated, it can grow through the wall of your bowel and spread to other parts of your body.
Symptoms of bowel cancer
Bowel cancer is often painless in the early stages, but there are symptoms, including:
- blood in your faeces, which may be mixed into your faeces or appear as flecks on the surface, or you may see it in the toilet or on toilet paper – get into the habit of looking into the toilet before flushing
- persistent changes in your bowel habit for several weeks – especially going to the toilet more often or having diarrhoea
- weight loss without any obvious reason and/or loss of appetite
- tiredness or breathlessness for no apparent reason – this may be caused by the small amount of blood loss from your bowel, resulting in anaemia (when there are too few red blood cells or not enough haemoglobin in your blood)
- pain, or a lump or swelling in your abdomen (tummy)
These symptoms aren't always due to bowel cancer. However the symptoms shouldn’t be ignored so if you have them, see your GP. If bowel cancer is caught early there is a better chance of curing it.
Causes of bowel cancer
The causes of bowel cancer aren't fully understood at present. One of the main factors is increasing age – more than eight out of 10 people diagnosed with bowel cancer are over 60.
Your risk of bowel cancer also increases if you have:
- a family history of bowel cancer
- one of two inherited bowel conditions that increase your risk – familial adenomatous polyposis (FAP) or hereditary non-polyposis colorectal cancer (HNPCC), also known as Lynch syndrome
- a long-term bowel condition, such as Crohn's disease or ulcerative colitis
- a diet that is low in fibre and fruit and vegetables and high in red and processed meats
- an inactive lifestyle, or are obese
- diabetes
Diagnosis of bowel cancer
Your GP will ask about your symptoms and examine you. He or she may also ask you about your medical history. Your GP may refer you to a doctor or surgeon who specialises in colorectal disease.
Tests for bowel cancer include the following.
- A colonoscopy, which is a test that allows a doctor to look inside your large bowel. The test is done using a narrow, flexible, tube-like telescopic camera called a colonoscope.
- A sigmoidoscopy, which is a procedure used to look inside your rectum and the lower part of your bowel.
- A barium enema, which involves placing a fluid containing barium (a substance which shows up on X-rays) into your bowel via your rectum. X-ray images of your abdomen then show the inside of your bowel more clearly.
If your doctor diagnoses bowel cancer, you may need further tests to find the size and position of the cancer.
These tests may include:
- an ultrasound scan of your abdomen to see if the cancer has spread
- a CT scan to show the position of the tumour
- an MRI scan to show two- and three-dimensional pictures of your bowel
- a chest X-ray to check the health of your heart and lungs
- blood tests to assess your general health
Screening for bowel cancer
Screening is important for detecting bowel cancer in its early stages. The Department of Health has introduced a bowel cancer screening programme in England. Bowel cancer screening kits are sent to men and women aged between 60 and 69, although if you’re older you can also request a kit. There are different programmes running in the rest of the UK. Ask your GP whether the screening programme has started in your area.
The screening kit contains a faecal occult blood (FOB) test that can detect small amounts of blood in your faeces. The FOB test doesn’t diagnose bowel cancer, but the results show if you need to have your bowel examined.
You may choose to have regular screening if you:
- are over 60 years old
- have a close relative who has had bowel cancer
- have FAP, HNPCC, or other diseases of the bowel lining such as ulcerative colitis or Crohn's disease
Treatment of bowel cancer
The type of treatment you have will depend on the size of the tumour, its position and whether it has spread.
Surgery
Surgery is the most common treatment for bowel cancer.
If you have surgery, the part of your large bowel that contains the cancer will be removed and the two open ends joined together. Lymph nodes (glands found throughout your body that are part of your immune system) near your bowel are often removed because they are the first place the cancer usually spreads to.
Sometimes, depending on the location and size of the cancer that is removed, the two ends of your bowel can't be rejoined. If this happens, the opening nearest the beginning of your bowel will be brought out on to the skin surface of your abdomen. A colostomy is an opening of your large bowel onto the surface of your tummy (abdomen) and an ileostomy is an opening of your small bowel onto the surface of the abdomen. The opening of the bowel is known as a stoma.
A bag is worn over the stoma, which collects your bowel movements outside your body. Most people who have surgery don't need a colostomy, but if you do, it's usually temporary.
If you have cancer in your rectum, you may need surgery to remove the part of your rectum that contains the cancer, as well as the fatty tissue and lymph nodes around your rectum. You’re more likely to need a colostomy if you have cancer of the rectum than if you have cancer of the colon.
Non-surgical treatments
Chemotherapy and radiotherapy
Sometimes it's not possible to remove all the cancer by surgery, so you may need to have additional treatment with chemotherapy and/or radiotherapy.
These treatments are given to destroy any remaining cancer cells and to prevent it spreading further. Chemotherapy and radiotherapy are also sometimes used to shrink the tumour before surgery or to kill any cancer cells that are left after surgery.
Chemotherapy and radiotherapy can both have side-effects.
Monoclonal antibodies
Monoclonal antibodies (MABs) are medicines that are designed to recognise and target markers that are commonly carried by cancer cells. There are three main MAB treatments for bowel cancer:
- bevacizumab
-
cetuximab
- panitumumab
These medicines seek out cancer cells and stop them growing. They are sometimes used alongside chemotherapy. They can be used for various stages of cancer – ask your doctor for more advice.
Prevention of bowel cancer
There is evidence that taking the following steps can help to reduce your risk of getting bowel cancer.
- Exercise for at least 30 minutes, five times a week.
- Eat five or more portions of fruit and vegetables every day.
- Cut down on the amount of processed and red meat you eat.
- Maintain a healthy weight.
- Eat foods high in fibre such as wholegrain bread, cereals and pasta.
- If you smoke, quit.
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email.
Why are people with bowel conditions such as Crohn's disease and ulcerative colitis at a higher risk of developing bowel cancer?
Can calcium help reduce the risk of developing bowel cancer?
What is the difference between a colostomy and an ileostomy?
Why are people with bowel conditions such as Crohn's disease and ulcerative colitis more likely to develop bowel cancer?
Inflammatory bowel diseases such as Crohn's disease and ulcerative colitis are thought to cause prolonged damage to your bowel over a long period of time which could result in bowel cancer.
Explanation
Crohn's disease and ulcerative colitis are both chronic diseases that cause your bowel to become inflamed. A chronic illness is one that lasts a long time, sometimes for the rest of your life. When describing an illness, the term chronic refers to how long a person has it, not to how serious a condition is.
It's thought that over time the damage caused to the lining of your bowel increases the risk of cancerous cells developing. If you have had Crohn's disease or ulcerative colitis and it has affected your entire bowel for more than eight years or affected the left side of your bowel for more than 15 years, then you’re at a higher risk of bowel cancer than the average person. It has been estimated that bowel cancer is caused by ulcerative colitis in about one in every 100 people diagnosed with bowel cancer.
If you have Crohn’s disease or ulcerative colitis and are at a higher risk of bowel cancer, it’s important that you’re screened regularly. If you have had your condition for between 10 and 20 years, it's recommended that you should be screened every three years. When you have had it for between 20 and 30 years this will be increased to every two years. After 30 years you will be screened every year. Your doctor will advise you on what is recommended and why.
Screening involves having a colonoscopy. A colonoscopy is a test that allows a doctor to look inside your large bowel. The test is done using a narrow, flexible, tube-like telescopic camera called a colonoscope. This type of screening means that if you do develop bowel cancer, it can be detected and treated early.
If you have any questions about Crohn's disease, ulcerative colitis or bowel cancer, talk to your doctor.
Further information
Macmillan Cancer Support
0808 808 00 00
www.macmillan.org.uk
National Bowel Cancer Screening Programme
www.cancerscreening.nhs.uk
Sources
- High risk groups for bowel cancer. Cancer Research UK. www.cancerhelp.org.uk, accessed 14 September 2009
- Who is screened for bowel cancer. Cancer Research UK. www.cancerhelp.org.uk, accessed 14 September 2009
- British Society of Gastroenterology. Guidelines for colorectal cancer screening in high risk groups. Gut 2002; 51:1-28.
Can calcium help reduce the risk of developing bowel cancer?
Possibly. Research has suggested that people who have more calcium in their diet are less likely to develop polyps in their bowel. These polyps may lead to the development of bowel cancer. However no research has directly shown that taking calcium supplements has any effect on your risk of getting bowel cancer.
Explanation
Calcium is an important part of your diet. It helps build strong bones and teeth, regulates your muscle contractions (including your heartbeat) and makes sure your blood clots normally. More recently, research has suggested that it may also help prevent certain cancers, including bowel cancer.
Studies have found that people who have high amounts of calcium in their diet may be less likely to develop bowel cancer than those who have little calcium in their diet. On average, adults need about 700mg of calcium per day. The research found that taking 1200mg of calcium supplements a day helps to prevent polyps (growths) developing in your large bowel. These polyps are dangerous because over time they can change and become cancerous.
So far, these findings have only shown that calcium supplements may contribute to the prevention of bowel polyps. More research needs to be done to establish whether increasing calcium in your diet prevents bowel cancer.
It's important to make sure that you’re getting enough calcium in your diet to keep you healthy and prevent long-term health conditions. Good sources of calcium include milk, cheese and other dairy products, green leafy vegetables (such as broccoli), soya products, nuts and anything made with fortified flour, and sardines and pilchards.
At this stage, it’s too early to say whether extra calcium in your diet will help protect against bowel cancer. However, there is evidence to show that taking the following steps will reduce your risk.
- Exercise for at least 30 minutes, five times a week.
- Eat five or more portions of fruit and vegetables every day.
- Cut down on the amount of processed and red meat you eat.
- Maintain a healthy weight.
- Eat foods high in fibre such as wholegrain bread, cereals and pasta.
- If you smoke, try to quit.
Further information
- Food Standards Agency
- Cancer Research UK
0808 800 40 40
www.cancerhelp.org.uk
Sources
- Dai Z, Xu YC, Niu L. Obesity and colorectal cancer risk: A meta-analysis of cohort studies. World J Gastroenterol 2007; 13(31):4199-206.
- Exercising for prevention. Beating Bowel Cancer. www.beatingbowelcancer.org, accessed 14 September 2009
- Eating for protection. Beating Bowel Cancer. www.beatingbowelcancer.org, accessed 14 September 2009
- Protecting against bowel cancer. Cancer Research UK. www.cancerhelp.org.uk, accessed 14 September 2009
- Weingarten M, Zalmanovici A and Yaphe J. Dietary calcium supplementation for preventing colorectal cancer and adenomatous polyps. Cochrane Database of Systematic Reviews 2008(3) www.cochrane.org
- Calcium. Food Standards Agency. www.eatwell.gov.uk, accessed 14 September 2009
What is the difference between a colostomy and an ileostomy?
A colostomy and ileostomy are both surgical procedures that involve bringing part of your bowel to your abdomen wall to create an artificial opening (stoma). The difference between them is in the part of the bowel that the stoma joins: a colostomy is when your large bowel is joined to the opening, whereas an ileostomy is when your small bowel is joined to the opening.
Explanation
Procedures with a name ending in 'ostomy' usually involve part of your bowel being joined to an artificial opening called a stoma in your abdomen. The first part of the word refers to the part of the bowel affected, ie ‘col’ in the word colostomy refers to your colon (large bowel) and ‘ile’ in ileostomy refers to your ileum (small bowel). A bag is worn over the stoma to collect bowel movements. The stoma is usually placed low down on your abdomen so it's hidden under your clothing.
These procedures are carried out if parts of your bowel can't be re-joined after having surgery for conditions such as Crohn's disease, bowel cancer or diverticulosis. A colostomy is usually temporary when used after surgery for bowel cancer. An operation is normally carried out a couple of months after your initial treatment to rejoin your bowel and remove the stoma. This is called a stoma reversal. Occasionally, if your bowel can't be rejoined, the stoma is permanent.
Having a stoma can be both physically and mentally challenging. However, most people are able to carry on with their lives as they did before and participate in activities such as swimming. There are patient support groups available, such as the Colostomy Association and the Ileostomy and internal pouch support group that can provide support and advice on having a stoma.
If you have any questions or concerns about colostomy or ileostomy, talk to your surgeon, GP or nurse.
Further information
- The Colostomy Association
0800 328 4257
www.colostomyassociation.org.uk
- Ileostomy and internal pouch support group (IA)
0800 0184 724
www.iasupport.org
Sources
- What is a stoma? Ostomy Lifestyle. www.ostomylifestyle.org, accessed 14 September 2009
- If you need a colostomy for bowel cancer. Cancer Research UK. www.cancerhelp.org.uk, accessed 14 September 2009
Related topics
Bowel cancer
Colonoscopy
Crohn's disease
Healthy eating
Physical activity
Stoma care
Ulcerative colitis
Publication date: January 2010.
Bowel cancer factsheet
Visit the bowel cancer health factsheet for more information.
Related topics
Abdominal ultrasound
Barium enema
Bowel cancer surgery
Chemotherapy
Colonoscopy
Crohn's disease
CT scan
MRI scan
Radiotherapy
Stoma care
Type 1 diabetes
Type 2 diabetes
Ulcerative colitis
Virtual colonoscopy
X-ray
Further information
- Beating Bowel Cancer
0845 071 9300
www.beatingbowelcancer.org
- Bowel Cancer UK
0800 840 35 40
www.bowelcanceruk.org.uk
Sources
- High risk groups for bowel cancer. Cancer Research UK. www.cancerhelp.org.uk, accessed 14 September 2009
- The bowel. Cancer Research Uk. www.cancerhelp.org.uk, accessed 14 September 2009
- Practice guidance: bowel cancer. Royal Pharmaceutical Society of Great Britain. www.rpsgb.org.uk, accessed 14 September 2009
- About bowel cancer screening. Cancer Research UK. www.cancerhelp.org.uk, accessed 14 September 2009
- Bowel cancer. Medical Research Council. www.mrc.ac.uk, accessed 14 September 2009
- Symptoms of bowel cancer. Cancer Backup. www.cancerbackup.org.uk, accessed 14 September 2009
- Information about bowel cancer. British Society of Gastroenterology. www.bsg.org.uk, accessed 14 September 2009
- Dai Z, Xu YC, Niu L. Obesity and colorectal cancer risk: A meta-analysis of cohort studies. World J Gastroenterol 2007; 13(31):4199-206.
- How bowel cancer is diagnosed. Cancer Backup. www.cancerbackup.org.uk, accessed 14 September 2009
- Bowel cancer screening - the facts. NHS Cancer Screening Programmes. www.dh.gov.uk, accessed 14 September 2009
- Bowel screening: Scottish bowel screening programme. NHS Scotland. www.bowelscreening.scot.nhs.uk, accessed 14 September 2009
- Bowel Screening Wales. Bowel Screening Wales. www.wales.nhs.uk, accessed 14 September 2009
- Screening: colorectal screeening. National Cancer Screening Service. www.cancerscreening.ie, accessed 14 September 2009
- Which treatment for bowel cancer? Cancer Research Uk. www.cancerhelp.org.uk, accessed 14 September 2009
- Surgery for large bowel cancer. Cancer Backup. www.cancerbackup.org.uk, accessed 14 September 2009
- Chemotherapy and monoclonal antibodies. Beating Bowel Cancer. www.beatingbowelcancer.org, accessed 14 September 2009
- Cetuximab for the first-line treatment of metastatic colorectal cancer. 2009. National Institute for Health and Clinical Excellence (NICE)
- Exercising for prevention. Beating Bowel Cancer. www.beatingbowelcancer.org, accessed 14 September 2009
- Eating for protection. Beating Bowel Cancer. www.beatingbowelcancer.org, accessed 14 September 2009
- Protecting against bowel cancer. Cancer Research Uk. www.cancerhelp.org.uk, accessed 14 September 2009
Publication date: January 2010.
















