Breast cancer
This factsheet is for people who have breast cancer, or who would like information about it.
Breast cancer is a tumour in the breast that contains cancerous cells. A breast tumour is a lump created by an abnormal and uncontrolled growth of cells. It can either be malignant (cancerous) or benign (not cancerous). Nine out of 10 breast lumps are benign.
How cancer develops
About breast cancer
Symptoms of breast cancer
Causes of breast cancer
Diagnosis of breast cancer
Treatment of breast cancer
Prevention of breast cancer
How cancer develops
The information on the video provided does not constitute advice on diagnosis or the treatment for heart disease and such advice should always be sought from a doctor or another suitably qualified health professional.
About breast cancer
Breast cancer is the most common cancer in the UK. Each year, around 45,000 women and 300 men are diagnosed with breast cancer. Eight out of 10 women who develop breast cancer are over 50.
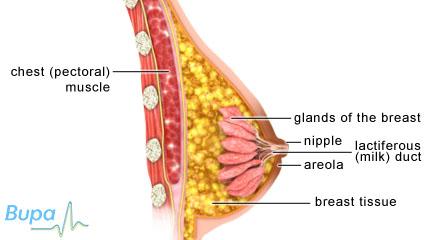
The breasts
Breasts are made up of fat, connective tissue and gland tissue divided into lobes. The lobes are connected to your nipple by ducts.
Most women have breasts of different sizes which look and feel different at certain times of the month, depending on their menstrual cycle. Your breasts also change during the different stages of your life, for example, after the menopause, they become less full or dense.
Breast tissue goes into your armpit where there are lymph nodes. These are glands that are part of your immune system.
Breast cancer usually starts in the cells lining the ends of the lobes and in the ducts themselves. It can spread from there into the breast tissue and lymph nodes.
Types of breast cancer
There are a number of different types of breast cancer, including some rare types, such as inflammatory breast cancer and Pagets disease. However, there are two main types of breast cancer. These are described below.
Non-invasive breast cancers
Non-invasive breast cancers are cancers that stay within the ducts or lobes of your breast and don’t spread to surrounding tissue or to other parts of the body. The most common type of non-invasive breast cancer is ductal carcinoma in situ (DCIS). This is a very early type of breast cancer where the cancer cells are only found inside the milk ducts and haven't spread into the breast tissue. In some cases, DCIS can develop into an invasive form of breast cancer.
Invasive breast cancers
Invasive breast cancers are cancers that have spread from the ducts or lobes of your breast into the surrounding tissue. The most common type of invasive breast cancer is called invasive ductal carcinoma (IDC), where the cancer cells are in the ducts and the breast tissue. Around eight out of 10 women diagnosed with breast cancer have this type. About one in ten women diagnosed with breast cancer have invasive lobular carcinoma (ILC), which starts growing in the lobes, but can spread to other parts of the breast. Both IDC and ILC can spread to other parts of the body.
Symptoms of breast cancer
Some women don't notice any changes in their breasts and breast cancer is found when they go for breast screening.
However, many women notice a breast lump or a change in the overlying skin or nipple. About nine out of 10 breast lumps aren’t cancer, but if you do find a lump, you should see your GP straightaway. There are also other symptoms to look out for:
- a change in the shape or size of your breasts
- a different shape to your nipple – for example, it may turn inwards or become irregular in shape
- dimpled skin
- a rash on or around your nipple
- blood-stained discharge from your nipple
- swelling or a lump in your armpit
These symptoms may be caused by problems other than breast cancer. If you have any of these symptoms, visit your GP for advice.
Causes of breast cancer
The cause of breast cancer isn't yet fully understood. However, there are certain factors that make developing breast cancer more likely. You’re more likely to develop breast cancer if you:
- are over 50 and have had either benign or malignant breast cancer before
- started your periods early or your menopause late
- have been exposed to radiation
- had a first pregnancy after the age of 30, or don't have children
- eat a lot of high-fat foods or drink more than the recommended limit of 14 units a week of alcohol
- are overweight and have been through the menopause
- have a close family member who has had breast cancer
- take the contraceptive pill or hormone replacement therapy (HRT), though this increased risk is small
Diagnosis of breast cancer
Your GP will ask about your symptoms and examine you. He or she may also ask you about your medical history and examine your breasts.
Your GP may refer you to a specialist breast clinic where you’re likely to have further tests. The most common tests are listed below.
- Ultrasound scan or mammogram. An ultrasound scan uses sound waves to produce an image of the inside of the body/or part of the body. This is usually done if you’re under the age of 35. A mammogram is an X-ray image of your breasts.
- Biopsy. Your doctor will take a small sample of tissue or cells. This will be sent to a laboratory for testing to determine the types of cells and if these are benign (not cancerous) or cancerous.
If you're found to have cancer, you may need to have other tests to assess if the cancer has spread. The process of finding out the stage of a cancer is called staging. The tests might include blood tests and a chest X-ray. Your doctor may also arrange for you to have a scan such as a CT (computerised axial tomography) or MRI (magnetic resonance imaging) scan. These scans produce images of the inside of your body and can help your doctor to see if the cancer has spread.
Treatment of breast cancer
There are a number of different treatments available for breast cancer and you may have more than one of them. The treatment you have will depend on a number of factors, such as whether or not you have been through the menopause, what type of cancer you have and how advanced it is, and whether your cancer has spread. Your doctor will talk to you about the treatments available to you.
Surgery
The first treatment for most people with breast cancer is usually surgery. Depending on the size and position of your breast lump, your surgeon may suggest either a lumpectomy or a mastectomy. A lumpectomy is where the lump is removed, usually with some healthy tissue around it. A mastectomy is where the whole of your affected breast is removed. You may be offered surgery to have your breast reconstructed afterwards.
With both of these procedures, some lymph nodes may also be removed from your armpit. This is to see whether the cancer has spread.
After surgery, you may have other treatments, such as radiotherapy. You will need radiotherapy if you have had a lumpectomy, but it’s less common after mastectomy. These treatments can help to reduce the chance of the cancer coming back or spreading.
Radiotherapy
Radiotherapy is a treatment to destroy cancer cells with radiation. A beam of radiation is targeted on the cancerous cells, which shrinks the tumour.
Radiotherapy is often used to treat breast cancer, usually after surgery. You’re likely to need a course of radiotherapy that lasts for three to five weeks. Radiotherapy is given as an out-patient treatment and each treatment only takes a few minutes but you will need to attend five days a week.
Chemotherapy
Chemotherapy uses medicines to destroy cancer cells. You may have chemotherapy:
- before your surgery – to shrink the tumour
- after surgery – to reduce the chance of cancer coming back or spreading
- as a treatment for breast cancer that has spread or come back
Some chemotherapy can be taken as a tablet, but most is given as an injection into your vein. You may need one or more different drugs as part of your treatment. You will usually have chemotherapy as a treatment cycle, with a few days taking the drugs and then a few weeks of rest afterwards. You may have a number of treatment cycles over a period of up to eight months.
Hormone therapy
Hormones, such as oestrogen, can affect the growth of breast cancer cells. Taking medicines that block these hormones can treat some kinds of breast cancer. Hormone therapies are usually used after you have had surgery, though they can be used before surgery or to treat cancer that has come back.
Women usually take hormonal treatments for at least five years following initial treatment for breast cancer. There are several types of hormone therapy. Your doctor will help you to choose the right medicine for you.
Biological therapies (monoclonal antibodies)
Biological therapy is treatment with a substance that stimulates your body to attack or control the growth of cancer cells. Antibodies are proteins produced by your immune system that usually fight against bacteria and viruses.
Monoclonal antibodies are made in a laboratory and are designed to seek out particular cells.
The most commonly used biological therapy is called trastuzumab (Herceptin). It works by targeting breast cancer cells that have a particular protein on their surface.
Trastuzumab is given into your vein via a drip. You will need to have it every three weeks for a year.
Not all women respond to treatment with biological therapies.
After your treatment
After your treatment has finished, your doctor will ask you to have regular check-ups. He or she will ask if you have any symptoms and may also arrange for you to have blood tests and mammograms. This is to check for signs of the cancer coming back.
If you’re well, you will need fewer check-ups as time goes on. If you have any symptoms in between your appointments or are worried at all, speak to your doctor.
Prevention of breast cancer
The NHS Breast Screening Programme invites all women between the ages of 50 and 70 for breast screening every three years. Breast screening means having a mammogram. This can help to show very early signs of any cancer.
You can also check your breasts regularly yourself. By being aware of how your breasts look and feel you can spot any changes quickly. See your GP if you notice any changes in your breasts.
Maintaining a healthy weight, breastfeeding, and not drinking excessive amounts of alcohol may help to protect against breast cancer.
Making sure you get enough vitamin D can reduce your risk of developing a number of cancers, including breast cancer. Vitamin D is produced naturally by your body when your skin is exposed to sunlight and can also be obtained from some foods, such as oily fish. However, most people don’t get enough from these sources. This is especially true if you live in a region that is nearer the North or South Pole than the equator (for example the UK, Canada or southern Argentina), where the sunlight to make vitamin D is only strong enough during the summer.
You can reduce your risk of developing breast cancer by taking 35 to 50 micrograms of vitamin D a day (about three to four high-strength, 12.5-microgram tablets). This will also reduce your risk of developing various bone-related conditions such as osteoporosis and osteomalacia. Always read the patient information leaflet that comes with your supplements and if you are pregnant or breastfeeding, ask your pharmacist or GP for advice first. Talk to your GP before taking vitamin D supplements if you are taking diuretics for high blood pressure or have a history of kidney stones or kidney failure.
Help and support
Being diagnosed with cancer can be distressing for you and your family. An important part of cancer treatment is having support to deal with the emotional aspects of living with cancer, as well as the physical symptoms. Specialist cancer doctors and nurses are experts in providing the support you need. You may also find it helpful to see a counsellor.
What is lymphoedema?
What is TNM staging for breast cancer?
How do I check my breasts for signs of breast cancer?
What is lymphoedema?
Answer
Lymphoedema is long-term swelling that can develop after treatment for breast cancer. It can develop on the side of your body where the breast cancer was, usually in your arm. Lymphoedema can’t be cured but you can manage the symptoms of it.
Explanation
Around one in five people who have treatment for breast cancer will develop lymphoedema.
After treatment for breast cancer, swelling can develop in your arm or on the side of your body where you had your treatment. Lymphoedema is long-term swelling.
Lymphoedema develops because the treatment you had for breast cancer can affect your lymph nodes and your lymphatic system. Surgery to remove lymph nodes or radiotherapy to the lymph nodes in your armpit can block the drainage channels of your lymphatic system. This means that fluid called lymph can’t drain properly and it begins to collect, which causes swelling.
Some things make the development of lymphoedema more likely, including:
- severe sunburn
- an infection following a cut or graze
- insect bites
- putting strain on your arm too soon after your treatment
In order to prevent lymphoedema, look after your skin, prevent cuts or grazes and carry out any exercises you have been given following your treatment.
If lymphoedema isn’t treated, it is likely to get worse. It can be painful and make movement difficult. You may also have dry and tight skin.
Lymphoedema can’t be completely cured but you can manage the symptoms of it, such as swelling and pain. Treatments include keeping your arm elevated, bandaging, exercise and massage.
If you notice any signs of swelling, talk to your doctor or nurse for advice. There are specialist nurses who can advise on the prevention and treatment of lymphoedema.
Further information
-
Breakthrough Breast Cancer
08080 100 200
www.breakthrough.org.uk - Cancer Research UK
0808 800 4040
www.cancerhelp.org.uk
-
Lymphoedema Support Network
020 7351 4480
www.lymphoedema.org
Source
- Lymphoedema after breast cancer treatment. Cancer Research UK. www.cancerhelp.org.uk, published May 2009
What is TNM staging for breast cancer?
Answer
The TNM staging system is a way for doctors to assess cancerous tumours. It's used to assess many different types of cancer, including breast cancer, and helps doctors understand how advanced the cancer is. Staging is also important in deciding the best treatments to use.
Explanation
TNM staging is a commonly used system in the UK to assess breast cancer tumours. TNM stands for ‘tumour, nodes, metastasis.’ Staging helps your doctor to see how big the tumour is, whether the cancer has spread to your lymph nodes and whether it has spread to other parts of your body.
Your doctor will use the information found during your tests, for example your biopsy, to give your breast cancer an overall TMN grade. Your doctor can then help you to choose the right treatment for you.
'T' stages are numbered between one and four. They describe the size of your tumour and where in the breast it is. Details of the different stages are listed below.
- T1 – tumour is 2cm or less across
- T2 – tumour is between 2cm and 5cm across
- T3 – tumour is larger than 5cm across
- T4 – describes the location of the tumour:
- T4a – tumour is attached to your chest wall
- T4b – tumour is attached to your skin
- T4c – tumour is attached to both your skin and your chest wall
- T4d – tumour is inflamed and the skin over it is red, swollen and painful to touch
The N part of staging tells your doctor if your cancer has spread to your lymph nodes and if so by how much. Lymph nodes are glands throughout the body that are part of the immune system. Cancer is able to spread to other parts of your body through your lymph nodes. If your cancer is staged as N0 it means that the cancer has not spread to your lymph nodes. N1 to N3 are used to show that the cancer has spread to your lymph nodes and where in the nodes cancer has been found.
The M part of cancer staging tells your doctor whether your tumour has spread to other parts of your body. A staging of M0 means that there is no sign that the cancer has spread to other parts of your body. A staging of M1 means that the cancer has spread to other parts of your body as well as your breast and lymph nodes.
Your doctor will put all this information together to come up with an overall stage for your cancer. You may have seen this written on test forms and other notes made by your doctor, or your doctor may have talked to you about it. For example, T2 N0 M0 means that your tumour is between 2cm and 5cm and there is no evidence that is has spread to your lymph nodes or any other part of your body.
Having an overall stage for your cancer is important. It's used to try and predict how your cancer will develop and to plan your treatment.
If you have any questions or concerns about breast cancer or the TNM staging system, talk to your doctor.
Further information
-
Breast Cancer Care
0808 800 6000
www.breastcancercare.org.uk -
Breakthrough Breast Cancer
08080 100 200
www.breakthrough.org.uk -
Cancer Research UK
0808 800 4040
www.cancerhelp.org.uk
Source
- TNM breast cancer staging. Cancer Research UK. www.cancerhelp.org.uk, published May 2009
How do I check my breasts for signs of breast cancer?
Answer
There is no specific examination that you can do yourself to check for signs of breast cancer. However, being breast aware and knowing what your breasts look and feel like will help you to spot any potential problems early on.
Explanation
Being breast aware means getting into the habit of checking the look and feel of your breasts on a regular basis. If you know what your breasts look and feel like, you will be able to spot any changes straightaway.
Check yourself in a way that is comfortable and convenient for you. You may find it easiest to check your breasts when you’re having a bath or shower or when you’re getting dressed in the morning. Using a mirror can make it easier to see your breasts from different angles. It’s also important to make sure you check the whole of your breast area including under your arm and at the top of your chest.
If you feel uncomfortable or anxious about checking your breasts, you may find it helpful to discuss your worries with your GP or a nurse.
When you’re feeling your breasts, check for the following:
- a lump, either in the breast or under your arm
- any area where the breast tissue feels like it’s thickened
- any unusual pain or discomfort
When you’re looking at your breasts, you’re checking for the following:
- a change in size or shape of your breasts (after puberty), for example one breast becoming larger or lower
- skin changes such as puckering or dimpling (skin looks like the texture of orange peel)
- a rash or crusting on the nipple or surrounding area
- nipple changes, such as a change in the position of your nipple, or a newly inverted (turned-in) nipple
- discharge from one or both nipples (unless you’re breastfeeding and it's milky discharge)
If you notice any of these changes, you should see your GP straight away. It's important to remember that every woman's breasts are different and that changes to your breasts aren’t always a cause for concern. They can be related to your menstrual cycle, age, pregnancy, the menopause and taking the contraceptive pill.
The NHS runs a national breast screening programme which offers a mammogram once every three years to women between the ages of 50 and 70. If you’re eligible for breast screening, it's important that you attend your appointments.
If you have any questions or concerns about checking your breasts or breast cancer, talk to your GP.
Further information
-
Breast Cancer Care
0808 800 6000
www.breastcancercare.org.uk -
Breakthrough Breast Cancer
08080 100 200
www.breakthrough.org.uk - Cancer Research UK
0808 800 4040
www.cancerhelp.org.uk
Sources
- NHS Breast Screening Programme. www.cancerscreening.nhs.uk, accessed 26 January 2010
- Signs and symptoms. Breakthrough Breast Cancer. www.breakthrough.org.uk, accessed 28 January 2010
- Breast awareness. Breast Cancer Care. www.breastcancercare.org.uk, accessed 28 January 2010
Related topics
Related topics
- Breast awareness and screening
- Breast lumps
- Cancer – a general overview
- Chemotherapy
- CT scan
- Mammography if you don't have breast symptoms
- Mammography if you have breast symptoms
- Mastectomy
- MRI scan
- Radiotherapy
Further information
-
Breast Cancer Care
0808 800 6000
www.breastcancercare.org.uk
-
Breakthrough Breast Cancer
08080 100 200
www.breakthrough.org.uk
-
CancerHelp
0808 800 4040
www.cancerhelp.org.uk
Sources
- Breast cancer symptoms. Cancer Research UK. www.cancerhelp.org.uk, published April 2009
- Breast cancer statistics: key facts. Cancer Research UK. www.cancerresearchuk.org, accessed 21 January 2010
- Invasive ductal breast cancer. Cancer Research UK. www.cancerhelp.org.uk, published May 2009
- Simon C, Everitt H, Kendrick T. Oxford Handbook of General Practice. 2nd ed. Oxford: Oxford University Press, 2007:518
- Early and locally advanced breast cancer. Diagnosis and treatment. National Institute for Health and Clinical Excellence (NICE), May 2009. www.nice.org.uk
- Visiting a breast clinic. Breakthrough Breast Cancer. www.breakthrough.org.uk, accessed 26 January 2010
- Which treatment for breast cancer? Cancer Research UK. www.cancerhelp.org.uk, published May 2009
- Surgical guidelines for the management of breast cancer. Association of Breast Surgery at BASO 2009. doi: 10.1016/j.ejso.2009.01.008
- Types of breast cancer surgey. Cancer Research UK. www.cancerhelp.org.uk, accessed 26 January 2010
- About breast cancer radiotherapy. Cancer Research UK. www.cancerhelp.org.uk, accessed 26 January 2010
- Types of breast cancer hormone therapy. Cancer Research UK. www.cancerhelp.org.uk, accessed 26 January 2010
- Breast cancer follow up. Cancer Research UK. www.cancerhelp.org.uk, published May 2009
- NHS Breast Screening Programme. www.cancerscreening.nhs.uk, accessed 26 January 2010
- Pearce SHS, Cheetham TD. Diagnosis and management of vitamin D deficiency. BMJ 2010;340: 142-47.
- Vieth R, Bischoff-Ferrari H, Boucher BJ, et al. The urgent need to recommend an intake of vitamin D that is effective. Am J Clin Nutr 2007; 85(3):649-50. www.ajcn.org















