Crohn's disease

This factsheet is for people who have Crohn's disease, or who would like information about it.
Crohn's disease is an inflammatory bowel disease and can have both short- and long-term effects. It causes symptoms such as diarrhoea and abdominal pain. Crohn’s disease is a mild condition for some people, for others it may be severe.
About Crohn’s disease
Symptoms of Crohn’s disease
Complications of Crohn’s disease
Causes of Crohn’s disease
Diagnosis of Crohn’s disease
Treatment of Crohn’s disease
Living with Crohn’s disease
About Crohn's disease
Crohn’s disease affects about one in 1,000 people. It mostly affects young adults, although older people can also develop it. Crohn’s disease can also run in families and about one in five people with the condition will have a family member who also has it.
Crohn's disease isn't caused by an infection and can't be caught from someone else.
Crohn's disease is inflammation of the wall of your bowel. It can affect any part of your digestive system, from your mouth down through your stomach and bowel to your anus. However, it's most common in your small bowel or the first part of your large bowel. It may affect more than one area and leave unaffected areas in-between.
If you have Crohn’s disease, you will have inflammation and swelling in affected areas of your bowel and ulcers may form. These are similar to mouth ulcers and cause raw areas of the lining of your bowel, which can bleed. Your bowel wall can become thickened and this may cause blockages.
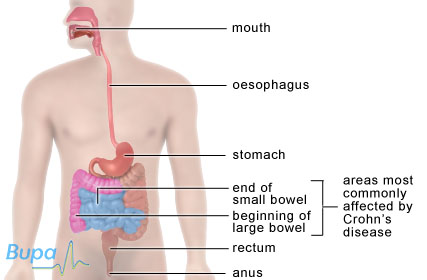
The areas of the bowel commonly affected by Crohn's disease
Crohn’s disease is a chronic illness. This means that it lasts for a long time, sometimes for the rest of the affected person’s life. The term chronic refers to how long a person has the illness, not to how serious a condition is.
Symptoms of Crohn’s disease
The symptoms of Crohn's disease can be unpredictable, with periods of time when the condition flares up and periods of time when there are few or no symptoms at all. The period when you have no symptoms is called remission. Usually there is nothing obvious that triggers the symptoms coming back (a relapse).
If you have a flare-up, the disease is said to be active. Symptoms include:
- diarrhoea – it may contain blood or mucus
- painful abdomen (tummy) – this often happens around an hour after eating
- weight loss
- fever
- tiredness
- bleeding from your rectum (back passage) – this may lead to anaemia, a condition when there are too few red blood cells or not enough haemoglobin in your blood
- tears, ulcers or abscesses (pus-filled areas) around your anus
Active Crohn's disease may cause other problems such as:
- mouth ulcers
- joint pain
- red, sore eyes
- rashes
Complications of Crohn’s disease
With severe, long-term inflammation, you may develop complications. The main complications are listed below.
- A fistula – this is an abnormal connection between two parts of your body. In Crohn’s disease, fistulas usually form between your bowel and your skin.
- An abscess in your abdomen – this is a collection of pus caused by an infection.
- A stricture – this can be caused by scar tissue that builds up after inflammation and may narrow and block your bowel.
If you have Crohn's disease that affects your large bowel (colon), you will have a higher risk of developing bowel cancer. One in 20 people with Crohn’s disease will develop bowel cancer in the 10 years after their condition is diagnosed.
Causes of Crohn’s disease
The reasons why you may develop Crohn's disease aren’t fully understood. It’s thought that you’re more likely to have Crohn’s disease if you have a reaction between your immune system (your body’s defence system) and certain bacteria in your bowel. For some people, Crohn’s disease may be inherited and passed down through families.
There are certain lifestyle factors which make developing Crohn’s disease more likely. For example, if you smoke, you’re more likely to develop Crohn's disease. The role of the foods you eat in causing Crohn's disease isn't fully understood. However, it's possible that you’re more likely to develop the condition if you eat only a small amount of fruit and vegetables.
Diagnosis of Crohn’s disease
Your GP will ask about your symptoms and examine you. He or she may also ask you about your medical history. You may be referred to a gastroenterologist, a doctor specialising in identifying and treating conditions of the digestive system. You may have a number of tests including:
- blood tests
- faeces (stool) tests
- colonoscopy – this allows a doctor to look inside your large bowel
- X-rays of your abdomen
- barium meal X-ray – this involves swallowing a drink containing barium (a substance which shows up on X-ray images) so the inside of your bowel can be seen more clearly
- CT scan or MRI scan
These tests are usually carried out as out-patient procedures. This means you have the test in hospital, but you won't need to stay overnight.
Treatment of Crohn’s disease
There is no cure for Crohn’s disease but your symptoms can be controlled.
Diet
There is no special diet for Crohn’s disease and it's important that you eat a healthy, balanced diet. However, if you have any blockages in your bowel which cause abdominal pain, you may want to eat foods that are low in fibre. This is called a low-residue diet. When your Crohn's disease is active, your doctor may recommend that you have a liquid diet, made up of simple forms of protein, carbohydrates and fats. This is called an elemental diet. This kind of diet helps your bowel to rest and reduces inflammation.
There is some evidence that fish oil supplements can help to reduce the number of flare-ups of Crohn’s disease.
Medicines
Medicines are the most effective treatment for most people with Crohn’s disease. Commonly used medicines are listed below.
- Aminosalicylates treat milder inflammation or reduce the chances of a flare-up.
- Corticosteroids, for example prednisolone, can help to reduce inflammation. These are very effective but can only be used for a short time during a flare-up because they can cause serious side-effects.
- Medicines to suppress your immune system, for example mercaptopurine or azathioprine, can help to reduce inflammation once you have stopped taking steroids.
- Antibiotics, for example metronidazole, can help to reduce bacteria in your bowel or treat abscesses.
If you have severe Crohn’s disease and have tried other treatments that haven’t worked, your doctor may suggest medicines called cytokine modulators.
If you need to take painkillers, you shouldn’t take non-steroidal anti-inflammatory medicines (NSAIDs), such as ibuprofen. These can cause a flare-up of Crohn’s disease. It's usually fine to take paracetamol as a painkiller, but check with your doctor first.
Surgery
Eight out of 10 people with Crohn’s disease may need to have an operation at some time. If you have a blockage or your bowel has become thickened, then you may need an operation to remove part of your bowel or to widen it. Surgery may also help if medicines aren’t able to control your condition.
Living with Crohn's disease
When your condition is in remission and you have few or no symptoms, then you will probably find that Crohn’s disease has little impact on your day-to-day life. However, when your condition flares up, your symptoms can make life more difficult. Symptoms such as diarrhoea and abdominal pain may mean you need to take time off work.
Once you start treatment for a flare-up, you should find that your symptoms get better quite quickly, usually after a few days or weeks.
Why are people with Crohn's disease more at risk of developing bowel cancer?
Is smoking linked to Crohn's disease?
If I have Crohn's disease, should I follow a special diet?
Why are people with Crohn's disease more at risk of developing bowel cancer?
Inflammatory bowel diseases like Crohn's disease are thought to cause prolonged damage to the cells lining your bowel. Over time, this can lead to bowel cancer. If you have had Crohn’s disease for longer than 10 years, you should have regular screening for bowel cancer.
Explanation
Crohn's disease is a chronic disease that causes your bowel to become inflamed. A chronic illness is one that lasts for a long time, sometimes for the rest of the affected person's life. When describing an illness, the term chronic refers to how long a person has had the illness, not to how serious a condition is.
It's thought that over time the damage caused to the lining of your bowel increases the risk of cancerous cells developing. The lining of your bowel has to be repaired again and again. This increase in the growth of cells may be what increases the risk of cancerous cells developing.
Some people with Crohn’s disease are more at risk than others of developing bowel cancer. You’re at greater risk if:
- you have had the condition for more than eight years
- Crohn’s disease started when you were a child or an adolescent
- You’re older than 45
- you have a family history of colon cancer
It's recommended that after you have had Crohn's disease for a certain length of time, you should be screened on a regular basis. Screening involves having a colonoscopy. A colonoscopy is a test that allows a doctor to look inside the large bowel. The test is done using a narrow, flexible, tube-like telescopic camera called a colonoscope. This type of screening means that if you do develop bowel cancer, it can be detected and treated early. You should have screening for bowel cancer:
- every three years if you've had Crohn's disease for between 10 and 20 years
- every two years if you've had Crohn's disease for between 20 and 30 years
- every year if you've had Crohn's disease for between 30 and 40 years
If you have any questions about Crohn's disease or bowel cancer, talk to your doctor.
Further information
-
National Association for Colitis and Crohn's Disease (NACC)
0845 130 3344
www.nacc.org.uk -
CancerHelp UK
0808 800 4040
www.cancerhelp.org.uk
Sources
- High risk groups for bowel cancer. Cancer Research UK. www.cancerhelp.org.uk, published October 2009
- Simon C, Everitt H, Kendrick T. Oxford handbook of general practice. 2nd edition. Oxford: Oxford University Press 2007:459
- Who is screened for bowel cancer? Cancer Research UK. www.cancerhelp.org.uk, published January 2010
Is smoking linked to Crohn's disease?
Yes. You’re more likely to develop Crohn's disease if you’re a smoker. If you have Crohn’s disease that affects your small bowel, then continuing to smoke means you’re likely to need more treatment than non-smokers or ex-smokers.
Explanation
Research has shown that if you smoke or have smoked, you’re more at risk of developing Crohn's disease than people who have never smoked. Exactly how or why smoking is linked to Crohn's disease isn’t fully understood.
People who continue to smoke after they have been diagnosed with Crohn's disease in their small bowel have more severe symptoms and are more likely to need stronger medicines to treat their condition Smokers are also more likely to need surgery and to relapse after surgery.
Stopping smoking is the best way to reduce your symptoms and the need for medicine or surgery. Stopping smoking also helps prevent other serious health conditions such as lung cancer or heart disease. Your GP will be able to give you support and advice about how to quit smoking.
If you have any questions or concerns about Crohn's disease or smoking, talk to your GP or doctor.
Further information
-
National Association for Colitis and Crohn's Disease (NACC)
0845 130 2233
www.nacc.org.uk
Sources
- Smoking and inflammatory bowel disease. National Association for Crohn’s and Colitis. www.nacc.org.uk, published May 2008
- Simon C, Everitt H, Kendrick T. Oxford handbook of general practice. 2nd edition. Oxford: Oxford University Press 2007:458
If I have Crohn's disease, should I follow a special diet?
The dietary advice for people with Crohn's disease is the same as for everyone else: follow a healthy, balanced diet. However, if you do find that a certain food makes your symptoms worse, find a substitute for it rather than cutting it out altogether (if possible). This will ensure that you don't lose whole food groups from your diet. Also, if you have active symptoms, you may find it helpful to follow a low-fibre diet.
Explanation
For most people with Crohn’s disease, there is no special diet that you should follow but it’s important that you eat a healthy, balanced diet. This can sometimes be difficult as you may find that certain foods or groups of foods make your symptoms worse.
Some food and drink can make symptoms worse, especially diarrhoea and bloating. These include:
- very hot or very cold foods
- unripe or dried fruit
- skin on fruit and vegetables
- spicy food
- fatty foods
- sugars in fruit (fructose)
- artificial sweeteners (sorbitol)
- caffeine (tea, coffee and cola drinks)
- alcohol
Try experimenting with food to find out what's right for you. If you suspect that a certain food or drink is causing symptoms, don't eat it for four to six weeks to see if your symptoms go away. Keeping a food diary of what you eat and what your symptoms are can be helpful in understanding triggers.
If you do identify a food that causes symptoms, try to find a substitute for it rather than just cutting it out completely. Cutting out foods can mean that you miss out an entire food group and the nutrients it provides. For example, if you find that eating butter causes symptoms, try switching to an olive oil-based spread instead.
Some people find that cutting out high-fibre foods can ease symptoms when they are having a flare-up. This may be because they are intolerant to fibre and continuing to have it in their diet makes their symptoms worse. High-fibre foods include wholegrain bread, brown rice and pasta, beans and peas, lentils, grains, seeds, fruit and vegetables.
Crohn’s disease can also affect how well your body is able to absorb vitamins and minerals from foods. This is another reason why it’s important to follow a balanced diet.
If you have any questions or concerns about Crohn's disease and diet, talk to your doctor or a dietitian.
Further information
-
National Association for Colitis and Crohn's Disease (NACC)
0845 130 2233[G1]
[G1]See comment G3[G1]
www.nacc.org.uk
Sources
- Crohn’s disease. British Society of Gastroenterology. www.bsg.org.uk,accessed 21 December 2009
- Managing bloating and wind. National Association for Crohn’s and Colitis. www.nacc.org.uk, published 2009
- Managing diarrhoea. National Association for Crohn’s and Colitis. www.nacc.org.uk, published July 2008
- Staying well with IBD. National Association for Crohn’s and Colitis. www.nacc.org.uk, published May 2008
Related topics
H2 Related topics
- Bowel cancer
- Bowel surgery for inflammatory bowel disease (IBD)
- Colonoscopy
- Hemicolectomy
- Iron-deficiency anaemia
- Irritable bowel syndrome
- Ulcerative colitis
H2 Further information
-
National Association for Colitis and Crohn's Disease
0845 130 2233
www.nacc.org.uk -
Core
020 7486 0341
www.corecharity.org.uk -
Crohn's in Childhood Research Association
020 8949 6209
www.cicra.org
H2 Sources
- Crohn’s disease. British Society of Gastroenterology. www.bsg.org.uk,accessed 21 December 2009
- Simon C, Everitt H, Kendrick T. Oxford handbook of general practice. 2nd edition. Oxford: Oxford University Press 2007:456
- Inflammatory bowel disease basics. National Association for Crohn’s and Colitis. www.nacc.org.uk, accessed 21 December 2009
- Guidance on the use of infliximab for Crohn’s disease. National Institute for Health and Clinical Excellence (NICE), May 2002. www.nice.org.uk
















