Echocardiogram
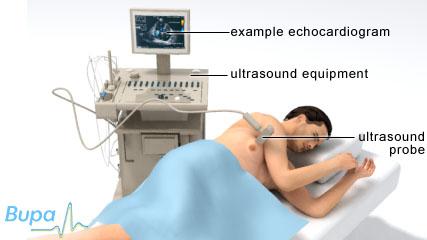
An echocardiogram uses ultrasound to produce moving, real-time images of your heart. The procedure helps to check the structure of your heart and how well it's functioning.
You will meet the doctor or technician carrying out your procedure to discuss your care. It may differ from what is described here as it will be designed to meet your individual needs. Details of the procedure may also vary from country to country.
About echocardiogram
What are the alternatives?
Preparing for an echocardiogram
What happens during a echocardiogram
What to expect afterwards
Recovering from an echocardiogram
What are the risks?
About echocardiogram
An echocardiogram (or echo) uses sound waves (known as ultrasound) to check the structure of your heart and how well it's working. The procedure involves a doctor or technician moving an ultrasound sensor over your chest to get pictures of your heart.
Echocardiograms can help to check how well your heart is pumping blood and can identify heart defects in adults, young children, newborn babies and unborn babies (fetal echocardiogram).
What are the alternatives?
Alternatives to an echocardiogram include the following.
• Transoesophageal echocardiogram. This is also an echocardiogram, but involves a doctor passing the ultrasound sensor into your oesophagus (the pipe that goes from your mouth to your stomach).
• Cardiac MRI scan. MRI is a special technique that uses powerful magnets, radiowaves and computers to produce detailed images (or scans) of the inside of your heart.
• Radionuclide test. In this test, a doctor injects a harmless, radioactive substance into your body. He or she then uses a special camera to take pictures of your heart. The radioactive substance shows up as it travels through your heart and your doctor uses this to assess your heart function and blood flow.
Please note that availability and use of specific tests may vary from country to country. Your doctor will advise you which procedure is most suitable.
Preparing for an echocardiogram
Echocardiograms are carried out in hospital by a cardiologist (a doctor specialising in conditions of the heart) or a sonographer (a technician trained in the procedure).
Your doctor will explain how to prepare for your procedure. For example, if you're having a stress echocardiogram you may be asked not to take beta-blockers or calcium-channel blockers for 48 hours and not to eat for two hours before the test.
What happens during an echocardiogram
An echocardiogram can take 30 to 45 minutes. You will be asked to undress to your waist and lie on your left-hand side. Your doctor or technician will place a clear gel over the left side of your chest. This is to make sure there will be a good, airtight contact between your skin and the sensor.
The sensor is held firmly against your skin and, as it moves across your chest, sends out sound waves and picks up the returning echoes. Pictures of the inside of your heart will be displayed on a screen. These pictures are constantly updated, so the scan can show movement. The test is painless but may feel uncomfortable when the sensor is being moved over your skin.
During the echocardiogram, you may be able to hear loud whooshing sounds. This is the sound of your blood flow and can be heard whether or not there are any abnormalities in your heart. Your heart rhythm will be also monitored throughout your echocardiogram.
FALTA IMAGEN
Stress echocardiogram
This is when the echocardiogram is done while your heart is under stress. This helps your doctor find out how well your heart copes when it has to work harder. You may be asked to do some exercise (such as walking on a treadmill or riding an exercise bike), or take medicines to make your heart beat faster and harder.
If you have an exercise stress echocardiogram, the exercise will be gentle at first but will get progressively more strenuous. Your doctor may take pictures of your heart while you are exercising or immediately afterwards.
If medicines are used to increase your heart rate, you may be asked to rest for 20 minutes after the test to make sure the effects have completely worn off.
Contrast echocardiogram
This is when a special dye (contrast agent) is injected into your vein during the echocardiogram. The dye helps show your heart more clearly. A contrast echocardiogram can help diagnose any holes in your hear
What to expect afterwards
The results of your echocardiogram may be discussed with you immediately after the examination. Alternatively, your results may be sent to your doctor who will discuss them with you at your next appointment.
Recovering from an echocardiogram
If you have an echocardiogram as an outpatient procedure, you will be able to return home after the test is completed. You will be able to continue with your day-to-day activities as usual.
What are the risks?
As with every procedure, there are some risks associated with an echocardiogram. We have not included the chance of these happening as they are specific to you and differ for every person. Ask your doctor to explain how these risks apply to you.
Side-effects
Side-effects are the unwanted but mostly temporary effects you may get after having the procedure. Medicines for stress echocardiograms can sometimes make you feel sick or dizzy.
Complications
Complications are when problems occur during or after the procedure.
- A standard echocardiogram is a safe procedure. There are no known complications associated with having it.
- A stress echocardiogram can occasionally cause heart rhythm problems, headache or chest pains.
- If contrast agent or medicines are used during the echo, there is a small risk of having an allergic reaction.
Speak to your doctor or technician for more information.
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email.
How will my doctor know if there is a problem with my heart?
What will happen after I get the results of my echocardiogram?
Why do I need a fetal echocardiogram?
How will my doctor know if there is a problem with my heart?
Answer
An echocardiogram is usually able to produce very detailed pictures of the structures inside your heart, helping your doctor to identify any problems.
Explanation
An echocardiogram can be used to look at the size, thickness and function of your left ventricle. This is one of the lower chambers of your heart, which pumps blood that contains oxygen around your body. Looking at the size of your left ventricle and how well it’s working can show your doctor whether there is a problem with your heart's pumping ability. Echocardiograms can also show any problems with your heart valves, the structures that help to control the way blood flows through your heart. Your doctor will look at the shape of the valves, how they are moving and whether they are calcified (have a build up of calcium deposits). This can show whether you have heart valve disease. Measuring how fast your blood is flowing will help your doctor to assess whether the valves have become narrowed or whether they are leaking.
An echocardiogram can also be used to look for other defects in the right side of your heart, as well as any problems with the artery that pumps blood to your body (aorta) or raised pressure in your lungs.
Further information
• British Cardiac Patients Association
01223 846845
www.bcpa.co.uk
• British Heart Foundation
0300 330 3311
www.bhf.org.uk
Sources
• Kumar P, Clark M, editors. Clinical medicine. Edinburgh: Elsevier, 2005:749–55
• Kasper DL, Braunwald E, Fauci A et al., editors. Harrison’s Principles of internal medicine., New York McGraw-Hill, 2005:1320–23.
What will happen after I get the results of my echocardiogram?
Answer
Your doctor will help you to choose the best course of action or treatment, based on the results of your echocardiogram together with any other tests you have had done.
Explanation
An echocardiogram is just one test that doctors use to assess how your heart is working. You may have other tests such as an electrocardiogram (ECG), a chest X-ray and blood and urine tests.
Your doctor may diagnose a problem with your heart using the results of all these tests. However, your echocardiogram may also rule out a problem with your heart, or show that you need further tests before a diagnosis can be made.
If tests do show up a problem with your heart, your doctor will discuss your treatment options with you. Depending on the problem identified, you may be advised to take medicine for your condition or to have surgery.
Further information
• British Cardiac Patients Association
01223 846845
www.bcpa.co.uk
• British Heart Foundation
0300 330 3311
www.bhf.org.uk
Source
• Tests. British Heart Foundation. www.bhf.org.uk, accessed 23 February 2010
H2 Why do I need a fetal echocardiogram?
Answer
A fetal echocardiogram is used to get a very detailed picture of your baby's heart, before your baby is born. It’s used to check whether your developing baby has a heart problem.
Explanation
If there's a problem with your baby's heart, it's often first noticed when you have your routine 20-week ultrasound scan.
You will be asked to have a fetal echocardiogram if a potential problem is seen during your routine 20-week scan, or if your obstetrician (the doctor who cares for you during pregnancy and childbirth) thinks there is a risk of a heart defect. Your baby may be more at risk of developing a heart problem if:
• you have a family history of congenital heart disease (heart disease from birth), or you already have a child with heart problems
• your baby has an abnormal heart beat
• your baby has problems with the development of other organs
• you have type 1 diabetes
• you have had certain medicines during your early pregnancy, for example, some anti-epilepsy medicines can cause heart defects in a developing baby.
A fetal echocardiogram can show up abnormalities in the structure or function of the heart and problems with the heart rhythm. However, some heart problems can't be detected until after your baby is born.
It can be a worrying time if you have been told you need a fetal echocardiogram. You can discuss the results fully with your specialist.
Further information
• Tiny Tickers
www.tinytickers.org
Sources
• Screening in pregnancy. Tiny Tickers. www.tinytickers.org, accessed 23 February 2010
• Fetal echocardiography. American Heart Association. www.americanheart.org, published October 2008
Related topics
• Echocardiogram
• Diagnosing heart conditions
Related topics
• Diagnosing heart conditions
• Electrocardiogram
• Transoesophageal echocardiogram
• Heart attack
• Heart failure
• Heart valve disease
Further information
• British Cardiac Patients Association
01223 846845
www.bcpa.co.uk
• British Heart Foundation
0300 330 3311
www.bhf.org.uk
Sources
- Echocardiogram. British Heart Foundation. www.bhf.org.uk, accessed 17 February 2012
- Clinical indications for echocardiography. British Society of Echocardiography. www.bsecho.org, published 2009
- Guidelines, protocols and patient information. British Society of Echocardiography. www.bsecho.org, accessed 17 February 2012
- Chaubal NG, Chaubal J. Fetal echocardiography. Indian J Radiol Imaging 2009; 19(1):60–68. doi: 10.4103/0971-3026.44524
- Screening. Tiny Tickers. www.tinytickers.org, accessed 17 February 2012
- Heart failure – chronic. Prodigy. www.prodigy.clarity.co.uk, published November 2010
- Heart failure. British Heart Foundation. www.bhf.org.uk, accessed 18 February 2012
- Ejection fraction heart failure measurement. American Heart Association. www.heart.org, published June 2011
- Aortic stenosis assessment. Stanford University. www.stanford.edu, published July 2009
- Radionuclide tests. British Heart Foundation. www.bhf.org.uk, accessed 20 February 2012
Produced by Krysta Munford, Bupa Health Information Team, April 2012.