Jaw joint dysfunction (tempromandibular dysfunction)
This factsheet is for people who have jaw joint dysfunction (temporomandibular dysfunction), or who would like information about it.
Jaw joint dysfunction can cause headaches, facial pain and/or jaw clicking. Jaw joint problems are common, but usually get better quickly with the right treatment.
About jaw joint dysfunction
Symptoms of jaw joint dysfunction
Causes of jaw joint dysfunction
Diagnosis of jaw joint dysfunction
Treatment of jaw joint dysfunction
About jaw joint dysfunction
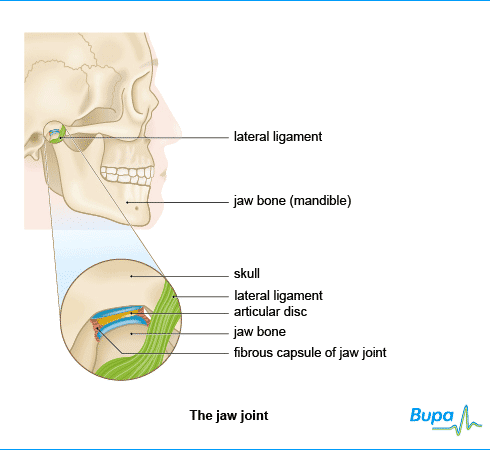
The jaw joints are where your lower jaw bone (mandible) meets your skull. The medical name for the jaw joint is the temporomandibular joint (TMJ). You have two jaw joints, one on each side, just in front of your ears. The joints allow you to open and close your mouth, and move it from side to side or backwards and forwards.
The joint is made up of part of the surface of each bone – the jaw and the skull – surrounded by a capsule. One side of the capsule is made of a ligament called the lateral ligament. Between the two bones is a disc of fibrous tissue which helps your jaw to move smoothly.
The jaw joint is one of the most complicated joints in your body, with a complex arrangement of muscles and ligaments allowing the different movements. Any problem that stops the muscles, ligaments, discs and bones from working properly together can cause a painful condition called temporomandibular dysfunction (TMD) or jaw joint dysfunction. It is also known as TMJ disorder.
Symptoms of jaw joint dysfunction
Your symptoms may include:
- pain – this is most likely to be an aching around your ear, and possibly in your cheek bone or neck, and it often relates to the muscles which control the jaw joint
- headache
- clicking and/or cracking noise (crepitus) in your jaw joint when you move it
- jaw locking
- stiffness, or being unable to open your mouth properly (trismus)
- a change in the way your teeth fit together when your jaw is closed
Your symptoms may be worse when you chew or yawn. They may also be worse if you are stressed.
Causes of jaw joint dysfunction
There are three main causes of jaw joint dysfunction. These are:
- Muscle pain and tension in your face (myofacial pain). Common causes include grinding or clenching your teeth (bruxism), especially at night, biting your nails, holding things between your teeth, stress or injury.
- Jaw misalignment (internal derangement). This means your jaw is not properly aligned with your skull, so the joint does not work smoothly. This can happen when the articular disc (thin disc within the joint) is in the wrong position, you have had a dislocated jaw, or your jaw joint has been injured.
- Degeneration of the joint. This is when the jaw joint is affected by arthritis, which happens most commonly in older people. Arthritis can also be caused by injury.
Injuries that can trigger jaw joint dysfunction include knocks to your jaw or overstretching when yawning, or during dental treatment.
Clicking is caused when the cartilage disc within the joint moves forwards out of its usual position when you open your mouth – the clicking is made when it moves back into place as you close your mouth. The noise may seem louder to you because the joint is close to your ear. Your jaw may lock if the cartilage does not return to its usual position after slipping out of place.
Diagnosis of jaw joint dysfunction
Your dentist will usually be able to diagnose jaw joint dysfunction by asking you about your symptoms and your medical and dental history.
Because the jaw joint is so complicated and there are many possible causes of jaw problems, it can be difficult to work out what is causing your symptoms. Your dentist will examine your jaw joint and look at your teeth for signs of wear due to grinding. This will involve checking the way that you open and close your mouth and feeling the muscles around the jaw to see if they are tender. Your dentist may also ask if you are stressed, because this can make grinding or clenching worse.
Treatment of jaw joint dysfunction
Treatment depends on the type of jaw joint problem you have.
Self-help
Your dentist will explain the problem to you and give you advice on anything you can do to reduce pain or clicking, such as stifling yawns and eating soft foods that don't need too much chewing.
He or she may recommend some exercises for you to do at home. It's important that you practise these as you have been shown.
Your dentist may also suggest using a heat pad such as a hot water bottle (filled with warm but not boiling water) wrapped in a cloth or towel.
If stress is causing your symptoms, you may find that relaxation therapy is helpful.
Medicines
You may find that over-the-counter painkillers such as paracetamol or ibuprofen help ease the pain. Always read the patient information that comes with your medicine and if you have any questions, ask your pharmacist for advice.
Non-surgical treatment
If your dentist thinks that you are clenching or grinding your teeth at night then he or she may offer a bite splint. This is a cover made from hard or soft plastic that fits over your upper or lower teeth and stops them coming into contact. You will probably need to wear this in the evenings and at night for four to six weeks before your dentist is able to see if it has made any improvement. You may notice a reduction in pain sooner than this.
These measures will probably relieve your symptoms. But if they don't, your dentist may refer you to an oral surgeon. The specialist may prescribe stronger painkillers or other medicines to help relieve the pain. If necessary, he or she may give you a short-term prescription for medicines which are usually used to treat depression – this is because some antidepressants also cause your muscles to relax.
Surgery
In a few, rare, cases your oral surgeon may recommend an operation on your jaw joints. However, it's important to talk through all of the options with him or her before going ahead with any surgery.
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email.
Can I get arthritis in my jaw?
Can physical therapy help to reduce the pain of jaw joint dysfunction?
Are there any drugs that I can take to help with my jaw joint problems?
Can I get arthritis in my jaw?
Answer
Yes, it's possible to get arthritis in your jaw joints (temporomandibular joints), but it’s very unlikely.
Explanation
Arthritis is a condition that causes inflammation (swelling) of your joints. There are several different types of arthritis. The most common types are osteoarthritis and rheumatoid arthritis. Both osteoarthritis and rheumatoid arthritis can affect your jaw joints, but this is very rare. It's also possible to get infectious arthritis in your jaw joints.
Osteoarthritis causes the cartilage in your joints to break down. This is more common in older people. If you have osteoarthritis in your jaw, you may experience a pain when you open and close your mouth, and clicking popping sounds or cracking sounds. If this happens, you should see your dentist or GP for advice.
Rheumatoid arthritis happens when your body’s defence system starts to attack its own cells, causing inflammation. Rheumatoid arthritis can affect your jaw joints.
Infectious arthritis can be caused if an infection in another area of your body, usually your head or neck, spreads to your jaw, but this is rare. Symptoms of infectious arthritis in your jaw are swelling, redness, pain on one side, and difficulty opening your mouth. You should see your dentist or GP if you have these symptoms.
Further information
Arthritis Care
www.arthritiscare.org.uk
H3 Sources
- TMJ disorders. National Institute of Dental and Craniofacial Research. www.nidcr.nih.gov, accessed 19 November 2009
- About arthritis. Arthritis Care. www.arthritiscare.org.uk, accessed 19 November 2009
- Atsu SS, Ayhan-Ardic F. Temporomandibular disorders seen in rheumatology practices: a review. Rheumatol Int 2006;26:781–87
Can physical therapy help to reduce the pain of jaw joint dysfunction?
Answer
Yes, physical therapy can help to improve the symptoms of temporomandibular dysfunction. Ask your dentist whether physical therapy would be a suitable treatment for you.
Explanation
There are several types of physical therapy which may be helpful for jaw joint dysfunction.
Ultrasound therapy uses sound waves to apply heat to the painful area. Heat helps to improve your circulation and reduce the pain in your muscles.
Spray and stretch exercises can be helpful. Your dentist or physiotherapist sprays a cooling substance over your cheeks and temples, which allows him or her to stretch your jaw muscles.
Further information
British Dental Health Foundation
0845 063 1188
www.dentalhealth.org.uk
Sources
- Atsu SS, Ayhan-Ardic F. Temporomandibular disorders seen in rheumatology practices: a review. Rheumatol Int 2006; 26:781–87
- Beers MH, Fletcher AJ, Porter R, et al, The Merck manual of medical information. New York: Pocket Books, 2003:685–90
Are there any medicines that I can take to help with my jaw joint problems?
H3 Answer
Yes, drug therapy can be helpful for some people.
Explanation
Taking painkillers that you can buy over the counter, such as paracetamol and ibuprofen, should help to relieve the pain. Always read the patient information leaflet that comes with your medication and if you have any questions, ask your pharmacist for advice.
If you're in a lot of pain, your dentist may prescribe a muscle-relaxing drug to help reduce the tightness and pain in your jaw. Another option for pain relief is an antidepressant, taken at a lower dose than that used to treat depression.
If your jaw joint dysfunction is related to anxiety, your dentist may prescribe you a drug called diazepam which relaxes your muscles and can also reduce anxiety. Your dentist will usually only prescribe this if you're in a lot of pain, and you can only take it for a short time.
Further information
British Dental Health Foundation
0845 063 1188
www.dentalhealth.org.uk
Sources
- Atsu SS, Ayhan-Ardic F. Temporomandibular disorders seen in rheumatology practices: a review. Rheumatol Int 2006; 26:781–87
- Joint Formulary Committee, British National Formulary. 57th ed. London: British Medical Association and Royal Pharmaceutical Society of Great Britain, 2009:189
- TMJ Disorders. National Institute of Dental and Craniofacial Research. www.nidcr.nih.gov, accessed 19 November 2009
- Simon C, Everitt H, Kendrick T. Oxford handbook of general practice. 2nd ed. Oxford 2005:912
Further information
-
British Dental Health Foundation
0845 063 1188
www.dentalhealth.org.uk -
British Dental Association
www.bdasmile.org
Sources
- TMD/TMJ (temporomandibular disorders). American Dental Association. www.ada.org, accessed 11 November 2009
- Atsu SS, Ayhan-Ardic F. Temporomandibular disorders seen in rheumatology practices: a review. Rheumatol Int 2006; 26:781–87
- Jaw joint problems. British Association of Oral and Maxillofacial Surgeons. www.baoms.org.uk, accessed 13 November 2009
- TMJ disorders. National Institute of Dental and Craniofacial Research. www.nidcr.nih.gov, accessed 13 November 2009
- TMJ dysfunction. GP Notebook. www.gpnotebook.co.uk, accessed 13 November 2009
- Simon C, Everitt H, Kendrick T. Oxford handbook of general practice. 2nd ed. Oxford University Press, 2006:913