Lung cancer
Published by Bupa’s Health Information Team, November 2010.
This factsheet is for people who have lung cancer, or who would like information about it.
Lung cancer is the second most common cancer and the third most common cause of death in the UK. About 33,400 people are diagnosed with lung cancer each year.
How cancer develops
About lung cancer
Types of lung cancer
Symptoms of lung cancer
Causes of lung cancer
Diagnosis of lung cancer
Treatment of lung cancer
Prevention of lung cancer
Help and support
How cancer develops
The information on the video provided does not constitute advice on diagnosis or the treatment for heart disease and such advice should always be sought from a doctor or another suitably qualified health professional.
About lung cancer
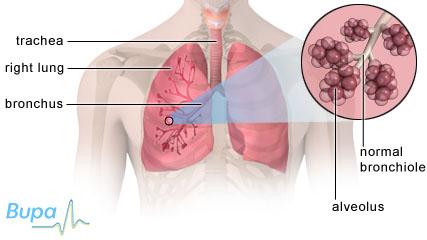
You have two lungs and they are located in your chest inside your ribcage. Your lungs bring oxygen into your body and pass it into your blood and remove carbon dioxide. Air passes from your nose and mouth into your windpipe (trachea). Your windpipe divides into two airways called the right and left bronchus, and one goes into each lung. Each bronchus divides into smaller tubes called bronchioles. These lead to air sacs called alveoli. This is where oxygen filters into and carbon dioxide filters out of your blood.
Lung cancer is the uncontrolled growth of cells in the lungs. This creates a lump (tumour) that can be either malignant (cancerous) or benign (not cancerous).
Lung cancer can start in the lining of your bronchi or your lung tissue – this is known as primary lung cancer. Cancer that has spread to the lungs through your bloodstream or your immune system from another part of your body is known as secondary lung cancer.
Types of lung cancer
There are two main types of lung cancer: non-small-cell (NSCLC) and small-cell (SCLC).
Non-small-cell lung cancer
About eight in 10 primary lung cancers are diagnosed as NSCLC. There are three types of NSCLC.
- Squamous cell carcinoma is the most common type of lung cancer and affects the bronchi.
- Adenocarcinoma mainly affects the outer part of your lungs and is the most common lung cancer in women and non-smokers.
- Large cell carcinoma can affect any part of the lungs and occurs in about one in 10 of all lung cancers.
It’s not always possible to identify the exact type of NSCLC you have and you may be diagnosed with ‘undifferentiated’ NSCLC. This won’t make any difference to your treatment as all NSCLC is treated the same way (see Treatment of lung cancer).
Small-cell lung cancer
This type of lung cancer starts in the smallest cells in your lungs – usually in the cells lining your bronchi. It can develop very fast and spread to other parts of the body very early – often before it’s been diagnosed. For this reason SCLC can be difficult to treat.
Symptoms of lung cancer
Most people with lung cancer have no early symptoms at all, but others may have:
- a cough – this can come on gradually
- a change in a cough you have had a long time – for example if you smoke, a constant dry cough may become chesty
- blood-stained phlegm (sputum)
- shortness of breath
- loss of appetite
- weight loss
- tiredness
Less common symptoms include:
- swelling of your face or neck
- a hoarse voice
- chest or shoulder pain
- broadening or thickening of the tips of the fingers (called clubbing)
These symptoms aren’t always caused by lung cancer but if you have had them for longer than three weeks, see your GP.
Causes of lung cancer
Smoking is the major cause of lung cancer, causing around nine in 10 lung cancers. Passive or second-hand smoking (breathing in other people’s smoke) is also linked to lung cancer.
Other factors that make lung cancer more likely include the following.
- Exposure to asbestos.
- Exposure to high levels of radon gas, a naturally occurring radioactive gas.
- Not enough fruit and vegetables in your diet.
- Previous lung disease.
- A weakened immune system, for example if you have HIV/AIDS.
Diagnosis of lung cancer
Your GP will ask you about your symptoms and examine you. He or she may also ask you about your medical history. Your GP will usually refer you to a hospital for a chest X-ray.
If your chest X-ray shows signs of lung cancer, you will usually be referred to a doctor who specialises in chest disease.
You may have the following tests to confirm diagnosis, find out the type of cancer you have and if the cancer has spread (this is called cancer staging).
- CT scan. This uses X-rays to make three-dimensional images of part of the body.
- Bronchoscopy. This is a procedure used to look inside your lungs. A narrow, tube-like, telescopic camera is passed down your windpipe into your lungs. Your doctor may remove a sample of tissue (a biopsy). This will be sent to a laboratory for testing to determine the type of lung cancer.
Treatment of lung cancer
Treatment of lung cancer depends on the type of cancer, how far it has spread and your general health.
SCLC is usually treated with chemotherapy because it has often spread by the time it’s diagnosed. NSCLC may be treated with surgery, chemotherapy, radiotherapy, laser treatment, or a combination of these methods.
Your doctor will discuss your treatment options with you.
Non-surgical treatments
- Radiotherapy uses radiation to destroy cancer cells. A beam of radiation is targeted on the cancerous cells, which shrinks the tumour. Radiotherapy is commonly given with chemotherapy, particularly in SCLC.
- Chemotherapy uses medicines to destroy cancer cells. It’s the main treatment in SCLC but can also be used in NSCLC. You may have it before or after surgery or with radiotherapy.
- Biological therapies are medicines that use substances occurring naturally in your body to kill cancer. The substances are manufactured so that they can be used in larger quantities to fight cancer. These include erlotinib (Tarceva), gefitinib (Iressa), cetuximab (Erbitux), and bevacizumab (Avastin).
- Radiofrequency ablation (or laser therapy) is when a high-energy beam of light is used to destroy cancer cells. It’s suitable if you have early stage NSCLC or you don’t want or can’t have surgery.
- Photodynamic therapy is when light-sensitive medicines are injected into your body and absorbed by the cancer cells. A low-powered laser is used to activate the medicines. This treatment is suitable if you have small early stage NSCLC, or when you don’t want or can’t have surgery.
Surgery
Surgery may be used to treat NSCLC if the cancer hasn’t spread. A small section, a lobe or a whole lung may be removed, depending on the size, type and position of the cancer. It also depends on how healthy your lungs are to start with.
Advanced lung cancer
Lung cancer can be difficult to cure because often it doesn’t cause symptoms until it has already spread. Where a cure isn’t possible, your treatment will aim to give you as good a quality of life as possible. This is known as palliative care.
You may be offered a combination of the treatments described here to help shrink the tumour and control your symptoms. Medicines are also available to help relieve other symptoms such as pain, cough, feeling sick and vomiting and poor appetite.
Prevention of lung cancer
You can reduce your risk of developing lung cancer by making certain lifestyle changes such as:
- stopping smoking
- not drinking excessive amounts of alcohol
- eating a balanced diet with at least five portions of fruit and vegetables a day
Making sure you get enough vitamin D can reduce your risk of developing a number of cancers, including lung cancer. Vitamin D is produced naturally by your body when your skin is exposed to sunlight and can also be obtained from some foods, such as oily fish. However, most people don't get enough from these sources. This is especially true if you live in a region that is nearer the North or South Pole than the equator (for example the UK, Canada or southern Argentina), where the sunlight to make vitamin D is only strong enough during the summer.
You can reduce your risk of developing lung cancer by taking 35 to 50 micrograms of vitamin D a day (about three to four high-strength, 12.5-microgram tablets). This will also reduce your risk of developing various bone-related conditions such as osteoporosis and osteomalacia. Always read the patient information leaflet that comes with your supplements and if you are pregnant or breastfeeding, ask your pharmacist or GP for advice first. Talk to your GP before taking vitamin D supplements if you are taking diuretics for high blood pressure or have a history of kidney stones or kidney failure.
Help and support
Being diagnosed with cancer can be distressing for you and your family. An important part of cancer treatment is having support to deal with the emotional aspects as well as the physical symptoms. Specialist cancer doctors and nurses are experts in providing the support you need, and may also visit you at home. If you have more advanced cancer, further support is available to you in hospices or at home.
I have heard that there are new treatments available for lung cancer. How can I find out if they are suitable for me and how can I benefit from them?
My doctor has mentioned hospice care. Can you tell me more about this?
I’m going to have surgery to remove part of one of my lungs. How will this affect my lifestyle – will I have to stop doing sports?
I have heard that there are new treatments available for lung cancer. How can I find out if they are suitable for me and how can I benefit from them?
A lot of new treatments for lung cancer are currently being tested in clinical trials. Ask your doctor for more information.
Explanation
New treatments for lung cancer are currently being tested in clinical trials. These are done to test if the new treatment is safe, has side-effects, is better than the current treatment available or helps you feel better.
Clinical trials may involve slight changes to treatments already being used or may involve completely new treatments. Some trials compare a standard treatment against a new one. You won’t be able to choose which treatment you receive – you will be given information about both and a computer will randomly allocate your treatment.
Another type of trial is a placebo-controlled trial. These are often done if there isn’t a good standard treatment available for you. Again, a computer will choose whether you receive a new experimental medicine or a dummy pill (placebo). The researchers will then see if either group of patients does better or has fewer side-effects. The advantage of entering a trial is that you may receive a new treatment or you may be helping patients in the future. All treatments used now have at sometime been tested in a clinical trial.
Ask your doctor if these treatments in clinical trials are suitable for you. He or she will consider the type and stage of your cancer, any treatment you have already had, your general health and other medical conditions you have.
Further information
-
Macmillan Cancer Support
0808 808 0000
www.macmillan.org.uk -
Cancer Research UK
0808 800 4040
www.cancerresearchuk.org
Sources
- How do you find a trial? Cancer Research UK. www.cancerhelp.org.uk, accessed 28 September 2010
My doctor has mentioned hospice care. Can you tell me more about this?
If you have cancer that can’t be cured and you need support to control your symptoms, your doctor may recommend hospice care.
Explanation
If you have cancer that can’t be cured, hospices can play an important role in offering you and your family support. Hospice care can improve your symptoms and quality of life. Many hospices also offer care if you aren’t terminally ill but if you would benefit from palliative care to help with symptoms such as pain, breathing problems and weight loss. You may not need full-time hospice care – you may only need to visit a hospice once a week for support or advice, or for a few days to get your symptoms under control.
Hospices also offer you and your family and friends a range of additional support. This includes counselling on how to cope with your cancer as well as bereavement support. You can find hospice care not only in specialist centres and palliative care units, but also in hospitals and hospice day centres.
Further information
-
Help the Hospices
www.helpthehospices.org.uk -
Macmillan Cancer Support
0808 808 0000
www.macmillan.org.uk
Sources
- What is hospice care? Help the Hospices. www.helpthehospices.org.uk, accessed 28 September 2010
- What is the difference between supportive care, palliative care and terminal care, or are they the same thing? Macmillan Cancer Support. www.macmillan.org.uk, accessed 28 September 2010
I’m going to have surgery to remove part of one of my lungs. How will this affect my lifestyle – will I have to stop doing sports?
The impact that surgery for lung cancer will have on your ability to do sport and exercise will depend on how much of your lung is removed and how healthy your lungs are.
Explanation
After surgery for lung cancer it’s important that you try to get yourself back to fitness as soon as possible. Before you leave the hospital ask your doctor or physiotherapist how much exercise you should try to aim to do. At first it’s important that you take it slowly and don’t over exert yourself.
As you start to recover from your surgery you could try brisk walking or swimming. This will improve your muscle strength and fitness. You could also try other exercises including breathing and relaxation techniques. Try to maintain a healthy lifestyle by not smoking, eating healthily and sensible drinking.
The impact surgery will have on lifestyle and ability to do sports will vary from person to person. It will partly depend on how much of your lung is removed and how healthy the rest of your lungs were before the surgery. If you are or were a smoker, your lungs may have been damaged. Your surgeon will have tested your lungs before surgery to identify this.
Further information
-
Macmillan Cancer Support
0808 808 0000
www.macmillan.org.uk -
Cancer Research UK
0808 800 4040
www.cancerresearchuk.org
Sources
- After surgery for lung cancer. Cancer Research UK. www.cancerhelp.org.uk, accessed 28 September 2010
- Lung cancer. The diagnosis and treatment of lung cancer. National Institute for Health and Clinical Excellence (NICE). Clinical Guideline 24, 2005. www.nice.org.uk, accessed 27 September 2010
- Complementary therapies. Macmillan Cancer Support. www.macmillan.org.uk, accessed 28 September 2010
Related topics
- Cancer – an overview
- Cancer staging and grading
Lung cancer factsheet
Visit the lung cancer health factsheet for more information.
Related topics
- Cancer – an overview
- Chemotherapy
- CT scan
- Giving up smoking
- Radiotherapy
- Cancer staging and grading
- X-ray
Further information
-
Macmillan Cancer Support
0808 808 0000
www.macmillan.org.uk -
Cancer Research UK
0808 800 4040
www.cancerresearchuk.org -
British Lung Foundation
0845 850 5020
www.lunguk.org
Sources
- Lung cancer. Cancer Research UK. www.cancerhelp.org.uk, accessed 27 September 2010
- Simon C, Everitt H, van Dorp F. Oxford handbook of general practice. 3rd ed. Oxford: Oxford University Press, 2010: 328–29
- Lung cancer – the diagnosis and treatment of lung cancer. National Institute for Health and Clinical Excellence (NICE). Clinical Guideline 24, 2005. www.nice.org.uk
- Lung cancer, oat cell (small cell). Emedicine. www.emedicine.medscape.com, accessed 5 October 2010