Osteoarthritis
Produced by Rebecca Canvin, Bupa Health Information Team, January 2012.
This factsheet is for people who have osteoarthritis, or who would like information about it.
Osteoarthritis is a condition that affects your joints, causing them to become stiff and painful. It usually develops gradually over a number of years and often affects the joints in your body that carry weight, for example knees, hips, feet and spine. However, osteoarthritis can also affect your fingers, the base of your thumbs, elbows and shoulders.
About osteoarthritis
Symptoms of osteoarthritis
Causes of osteoarthritis
Diagnosis of osteoarthritis
Treatment of osteoarthritis
Living with osteoarthritis
Video
About osteoarthritis
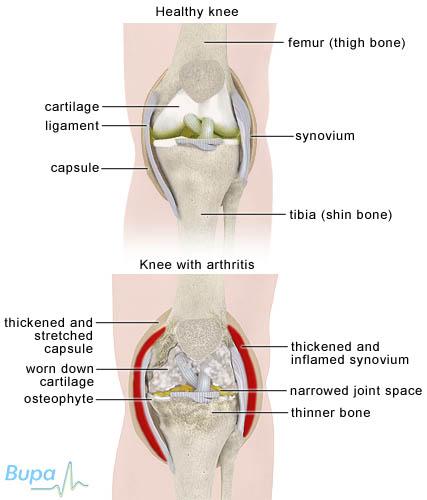
Osteoarthritis causes the cartilage on the end of your bones to get rougher and thinner. The bone underneath thickens and grows outwards, creating growths called osteophytes that can make your joint look knobbly. The capsule around the joint also thickens and tightens. Sometimes fluid also builds up and your joint can look and feel swollen.
These changes to your joints can cause pain and stiffness and make it more difficult for you to get around, or to do everyday tasks. Osteoarthritis can affect people in different ways. You may find that your osteoarthritis gets worse over a short period of time and causes a lot of damage to your joints, which significantly impacts your day to day life. Or, you may find that your condition develops slowly over many years, causing small changes to your joints that don't get any worse, or even ease over time.
Although there isn't a cure for osteoarthritis, there are many treatments and self-help measures that can ease your symptoms.
Osteoarthritis is most common in people over the age of 50, although it can develop in younger people. It's thought that worldwide, nearly one in 10 men and one in five women over 60 have symptoms of osteoarthritis.
Symptoms of osteoarthritis
When osteoarthritis first develops, you may have some stiffness and pain in your joint, which can get worse when you exercise or at the end of the day.
As your condition develops you may notice other symptoms. The main ones are listed below.
- A deep, aching joint pain. Depending on which of your joints is affected, you may find this pain spreads. For example, if you have osteoarthritis in your hip, you may have pain down the side or front of your thigh and into your buttock. This is called radiated pain.
- A reduction in your range of movement in the joint. This means you won't be able to move your joint into the positions you did before, or move them as far.
- A crunching and grinding sensation and noise in your joints when you move them. This is called crepitus.
- A change in the shape of your joint, with hard bony growths and soft swelling caused by extra fluid.
- Your joint may give way when you put weight through it. This can happen because your muscles have weakened or because your joint is less stable.
There may be times when your symptoms get worse, for example, when the weather changes and becomes damp, or when you have been more active than usual.
Causes of osteoarthritis
The exact cause of osteoarthritis isn't known. However, certain factors may increase your risk of developing the condition. You're more likely to develop osteoarthritis if:
- you're aged over 50
- you're overweight or obese
- one of your parents has the condition
- you have previously injured the joint
- you have rheumatoid arthritis or gout
Diagnosis of osteoarthritis
There is no single test that can check for osteoarthritis. Your doctor will ask about your symptoms and examine you. He or she may also ask about your medical history.
During the examination your doctor will look for bony growths and swelling and any creaking in your joint. He or she will also check how well your joint moves and how stable it is.
Occasionally your doctor may also arrange for you to have an X-ray of the affected joint. An X-ray can help to show whether the normal joint space is reduced because of a loss of the protective cartilage. It can also show if you have any extra bone growth around your joint or any roughening or thickening of the joint surface. Sometimes calcification of the cartilage can be seen (this is when calcium builds up in the joint). It can be a sign of a type of osteoarthritis that can quickly become severe and cause more severe pain from time to time.
Please note that availability and use of specific tests may vary from country to country.
Treatment of osteoarthritis
There is no cure for osteoarthritis. However, there are a number of treatments that can help you to manage the condition and control your symptoms.
Self-help
There are many things you can do to reduce the pain and stiffness in your joints, and to make day-to-day life easier. Self-help measures can help to reduce the stress on your joints and reduce the severity of your condition. Some of the main ones are listed below.
- Try to maintain a healthy weight for your height. This may mean losing weight if you're overweight, because it puts more stress on your joints and can make osteoarthritis worse.
- Exercise regularly and keep moving. Exercise can help to keep your joints working well but it's important to rest your joints as well. Doing a little exercise regularly may be helpful.
- Pace yourself. For example, spread out any chores that need doing, rather than trying to do them all at once.
- Use a walking stick to ease any stress on your knee or hip joint.
- Wear shoes with a soft, thick, cushioned sole. This will help to reduce any jarring.
- Massage the muscles around your joints affected by osteoarthritis to help ease pain.
- Use a heat pad or an ice pack to help ease pain. Don't put either of these directly onto your skin as they may cause burns – wrap them in a towel or dishcloth first.
- Think about making changes to your car, home or workplace to ease any stress on your joints. You may be able to get help from an occupational therapist (a health professional who can give practical assistance to help you manage with everyday tasks and increase your independence).
- Use braces or supports for your joints to keep your joint stable and provide support. Ask your doctor about these.
Medicines
Painkillers can help to ease pain and stiffness, but they can't make your condition better. Paracetamol (acetaminophen) may help for mild pain. You can also try non-steroidal anti-inflammatory (NSAIDs) creams and gels, such as ibuprofen and diclofenac. You can put these directly onto the joint affected by osteoarthritis. Always read the patient information leaflet that comes with your medicine and if you have any questions, ask your pharmacist for advice.
If these medicines don't work, your doctor may suggest taking NSAIDs as tablets rather than as a cream or gel. He or she may also suggest a stronger type of painkiller called opioids. If you're taking NSAID tablets regularly, your doctor may suggest taking a medicine called a proton pump inhibitor as well. This medicine protects your stomach and reduces the risk of side-effects from NSAIDs. Using NSAIDs for long periods has been linked with heart, kidney and stomach problems.
Capsaicin cream is made from pepper plants and is an effective painkiller, particularly if you have hand or knee osteoarthritis. It's only available with a prescription.
If you have a particularly painful, swollen joint, your doctor may suggest a steroid injection directly into the joint. This can only be done a few times each year, but can help to reduce inflammation and ease pain. The injection usually works within a few days or a week or so, and can last for weeks or months.
Non-surgical treatments
Transcutaneous electrical nerve stimulation (TENS) is an electronic device that sends pulses through your skin to your nerve endings. It interferes with the messages being sent to your brain and can help to relieve your pain. Some people with osteoarthritis find it useful, although it doesn't work for everyone.
You can buy a TENS machine from a chemist or drugstore. You may be able to loan one from a physical therapist (physiotherapist) to try, before you decide to buy one.
Surgery
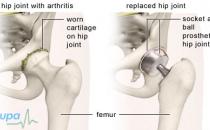
If you have osteoarthritis that causes severe pain, or which has a significant impact on your day-to-day life, your doctor may suggest an operation to replace the affected joint with an artificial one.
Complementary therapies
Many people with osteoarthritis take supplements or use complementary medicines to ease their symptoms.
Fish oils, such as cod liver oil, may be helpful in easing pain and stiffness. You need to take fish oils for between three and six months to see any benefit.
Glucosamine and chondroitin are two of the most commonly used supplements. Current research suggests that they don't work to reduce joint pain and they aren't recommended as treatments for osteoarthritis. However, some people with osteoarthritis do get benefit from taking them. If you decide to take glucosamine or chondroitin you will need to take them for up to two months before you will know if they work for you.
There is little evidence that other therapies, such as acupuncture, are effective at treating osteoarthritis. However, they may make you feel more relaxed, which may help you to manage your osteoarthritis. Speak to a doctor before trying complementary therapies or herbal remedies.
Availability and use of different treatments may vary from country to country. Ask your doctor for advice on your treatment options.
Living with osteoarthritis
Living with osteoarthritis can be difficult and the more severe your condition is, the bigger the impact it's likely to have on your life.
As with many long-term conditions that cause pain and discomfort, having osteoarthritis can affect your emotions and your relationships with those around you. It can also have an impact on your sleep, which may affect other areas of your life, or lead to depression. Talk to your doctor about the impact the condition has on your day-to-day life and what might be done to help you. You may also find it helpful to contact support groups and talk to other people living with osteoarthritis.
Video
See our videos about osteoarthritis, they include:
Should I exercise if I have arthritis?
What exercises can I do for arthritis in my hands, wrists and forearms?
What exercises can I do for arthritis in my shoulders?
What exercises can I do for arthritis in my back?
What exercises can I do for arthritis in my knees?
Published by Bupa's health information team, November 2009.
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email.
Will eating oily fish or taking fish oil supplements help osteoarthritis?
Answer
There isn’t any evidence to show that fish oils are helpful in improving osteoarthritis.
Explanation
Fish oils contain omega-3 polyunsaturated fatty acids. Some research has suggested that these fatty acids may have a beneficial effect in inflammatory forms of arthritis, including rheumatoid arthritis, reactive arthritis, psoriatic arthritis and ankylosing spondylitis. There is evidence to suggest that omega-3 fatty acids may help to reduce the inflammation associated with these forms of arthritis.
However, studies looking at the effect of fish oils on osteoarthritis have produced disappointing results and more research is needed.
Further information
Arthritis Care
0808 800 4050
www.arthritiscare.org.uk
Arthritis Research Campaign
0870 850 5000
www.arc.org.uk
Sources
- Diet and arthritis. Arthritis Research Campaign. www.arc.org.uk, accessed 18 June 2009
- Healthy eating and arthritis. Arthritis Care. www.arthritiscare.org.uk, accessed 18 June 2009
- Will cod liver oil protect me from osteoarthritis? Food Standards Agency. www.eatwell.gov.uk, accessed 18 June 2009
I don't like swimming. Is there another form of exercise that will help osteoarthritis?
Answer
Yes. A mix of different types of exercise is ideal. However, before you start, get advice from your GP, physiotherapist or occupational therapist so that an exercise programme can be tailored to your needs.
Explanation
When you’re in pain you may not feel like exercising but there are three types of exercise that can bring real benefits.
- Strengthening exercises target the muscles around affected joints and improve your stability. They can also help to reduce pain.
- Exercises that involve moving your joints through their full range of movement help you to stay flexible and improve your strength and posture. Slowly build up and increase how far you move your joints. Aim to do these exercises in each joint of your body every day.
- Aerobic exercise that increases your heart rate and makes you slightly out of breath can help reduce pain, and also improves your general health and wellbeing. Walking, cycling, dancing or everyday activities such as housework can help.
Some tips that may help you when exercising include the following.
- Make exercise part of your daily routine and build up slowly.
- Have a warm bath or shower, or place a hot water bottle on affected joints before exercising.
- Never force a painful joint. It’s common to feel some pain as you build up your exercise programme. However, if any pain lasts longer than two hours after exercising, contact your GP.
- Always wear cushioned and supportive footwear.
Further information
Arthritis Care
0808 800 4050
www.arthritiscare.org.uk
Arthritis Research Campaign
0870 850 5000
www.arc.org.uk
Sources
- Osteoarthritis. Arthritis Research Campaign. www.arc.org.uk, accessed 18 June 2009
- Keeping active. Arthritis Care www.arthritiscare.org.uk, accessed 18 June 2009
Can I take glucosamine if I have a shellfish allergy?
Answer
Generally no. Glucosamine is usually made from shellfish, so you shouldn’t take it if you’re allergic to shellfish.
Explanation
Some vegetarian versions of glucosamine are available that may be suitable if you have a shellfish allergy. It’s important to speak to your GP before taking any sort of glucosamine.
Glucosamine may provide some pain relief for people with osteoarthritis, although there is only limited evidence that it’s effective. If you have an allergy to shellfish, it's best not to take glucosamine at all. The supplement is made from shellfish shells. Some experts say shellfish allergy is caused by shellfish flesh rather than the shell, but it’s possible that you will have an allergic reaction to glucosamine if you have a shellfish allergy. Speak to your GP if you’re considering taking glucosamine.
The supplement chondroitin, often taken with glucosamine, isn’t made from shellfish. However, there is only limited evidence to show that chondroitin is effective in treating osteoarthritis.
Further information
The Anaphylaxis Campaign
01252 542029
www.anaphylaxis.org.uk
Arthritis Research Campaign
0870 850 5000
www.arc.org.uk
Sources
- Glucosamine – what are the adverse effects? National electronic Library for Medicines. www.nelm.nhs.uk, accessed 18 June 2009
- Common food allergens. The Anaphylaxis Campaign. www.anaphylaxis.org.uk, accessed 18 June 2009
- Complementary and alternative medicines for the treatment of rheumatoid arthritis, osteoarthritis and fibromyalgia. Arthritis Research Campaign, 2009. www.arc.org.uk
- Glucosamine and chondroitin in osteoarthritis. National Prescribing Service Limited. www.nps.org.au, accessed 24 July 2009
Related topics
Osteoarthritis
Psoriatic arthritis
Rheumatoid arthritis
This information was published by Bupa's health information team and is based on reputable sources of medical evidence. It has been peer reviewed by Bupa doctors. The content is intended for general information only and does not replace the need for personal advice from a qualified health professional.
Publication date: November 2009.
Osteoarthritis factsheet
Related topics
Acupuncture
Healthy eating
Herbal remedies
Hip replacement
Knee arthroscopy
Knee replacement
Non-steroidal anti-inflammatory drugs (NSAIDs)
Rheumatoid arthritis
Further information
Arthritis Care
0808 800 4050
www.arthritiscare.org.uk
Arthritis Research Campaign
0870 850 5000
www.arc.org.uk
Sources
- Chronic rheumatic conditions. World Health Organization, accessed 30 July 2012
- Living with osteoarthritis. Arthritis Care. www.arthritiscare.org.uk, published May 2011
- Osteoarthritis. Arthritis Research UK. www.arthritisresearchuk.org, published April 2011
- Osteoarthritis. eMedicine. www.emedicine.medscape.com, published July 2011
- Osteoarthritis. Prodigy. www.prodigy.clarity.co.uk, published August 2008
- Osteoarthritis. National Institute for Health and Clinical Excellence (NICE), February 2008. www.nice.org.uk
- Looking after your joints. Arthritis Research UK. www.arthritisresearchuk.org, accessed 10 August 2011
- Taking care of joints. Arthritis Care. www.arthritiscare.org.uk, published January 2011
- Exercise and arthritis. Arthritis Research UK. www.arthritisresearchuk.org, accessed 4 August 2011
- Exercise and arthritis. Arthritis Care. www.arthritiscare.org.uk, published April 2011
- Keeping active. Arthritis Care. www.arthritiscare.org.uk, published April 2011
- Splints for arthritis of the wrist and hand. Arthritis Research UK. www.arthritisresearchuk.org, published 2011
This information was published by Bupa’s health information team and is based on reputable sources of medical evidence. It has been peer reviewed by Bupa doctors. The content is intended for general information only and does not replace the need for personal advice from a qualified health professional.