Osteoporosis
This factsheet is for people who have osteoporosis, or who would like information about it.
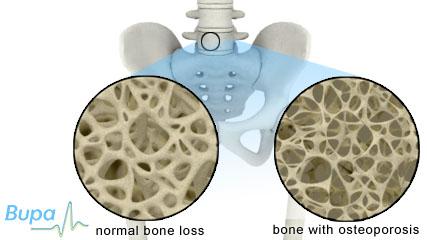
Osteoporosis literally means ‘porous bones’. It’s a condition where bones lose density causing them to become weak, brittle and more likely to break (fracture).
How osteoporosis develops
About osteoporosis
Symptoms of osteoporosis
Complications of osteoporosis
Causes of osteoporosis
Diagnosis of osteoporosis
Treatment of osteoporosis
Prevention of osteoporosis
How osteoporosis develops
About osteoporosis
About one in two women and one in five men over 50 will fracture a bone because of osteoporosis. Osteoporosis can affect all age groups, but it’s most common in post-menopausal women. Having osteoporosis doesn’t automatically mean that your bones will fracture; it just means that it’s more likely.
Symptoms of osteoporosis
You can’t see or feel your bones getting thinner, and may only become aware of the condition when you fracture a bone. Osteoporosis weakens the bones in your back (vertebrae), so other signs to look out for include back pain and any changes in your height.
Complications of osteoporosis
People with osteoporosis are more likely to fracture bones in the wrists, hip, pelvis and back. Fractures can, however, occur in any bone. They can result in pain, disability and loss of independence.
Causes of osteoporosis
Healthy bone consists of a strong mesh made of protein and minerals (particularly calcium). This mesh is living tissue that is constantly being renewed by two types of cells. One type (osteoblasts) builds up new bone and the other (osteoclasts) breaks down old bone. Up to our mid-20s our skeleton is strengthened, but from our 40s onwards our bones gradually lose their density as a natural part of ageing.
Our bone health is largely down to the genes we inherit from our parents. However, there are other factors that can put you at greater risk of osteoporosis.
- Gender – women in their late 40s and early 50s face the menopause. This means they lose the protective effects of the hormone oestrogen and are at higher risk of having osteoporosis.
- Race – Caucasian or Asian races are at greater risk than African-Caribbean people.
- Surgery – women who have a hysterectomy before the age of 45 (especially if both ovaries are removed) are at increased risk of osteoporosis.
- Previous bone injury – bone fractures make the bone weaker so affected bones lose their density quicker.
- Long-term immobility – bones and muscles become weak if your body isn’t active.
- Being underweight – if you’re underweight your body won’t have the essential nutrients it needs to repair bones and keep them strong.
- Poor diet – low levels of vitamin D or dietary calcium means your body can’t repair bones and keep them strong.
Some medicines and health conditions can increase your risk of osteoporosis.
- Long-term use of corticosteroids – used to treat severe allergies or inflammation.
- Aromatase inhibitors – used in breast cancer treatment.
- An overactive thyroid – such as hyperthyroidism or hyperparathyroidism.
- Rheumatoid arthritis.
- A decreased function of the testicles (hypogonadism) – low levels of testosterone in men increases their risk of osteoporosis.
- Digestive disorders – such as Crohn’s Disease, chronic liver disease or coeliac disease.
Diagnosis of osteoporosis
Osteoporosis is usually diagnosed in hospital, often after a fall or bone fracture.
Your doctor will measure your bone density using a DEXA scan. The scan is painless and takes 10 to 20 minutes. Osteoporosis is diagnosed if your bone density is found to be lower than average. If your bone density is slightly lower than average, it’s known as osteopenia.
You may also have other tests, such as a blood and urine tests, MRI scan or an X-ray to rule out other conditions or to understand what is happening with your bones. There is, however, no single blood test which will tell your doctor if you have osteoporosis.
Treatment of osteoporosis
Self-help
If you have osteoporosis you need to be careful of vigorous, high-impact exercise. However, leading an active lifestyle will improve your balance, coordination and develop muscle strength. This can reduce your risk of falling and fracturing a bone. Beneficial exercise includes swimming, gardening, walking, golf and Tai Chi.
It’s important to eat a diet that is rich in calcium to maintain healthy bones. Aim to take 1,000mg of calcium every day, either in your diet or as a supplement. Good sources of calcium include milk and dairy products, such as cheese and yogurt, dried apricots or figs and some green leafy vegetables such as broccoli and cabbage. Calcium tablets can be purchased at a chemist, but always ask your doctor before taking calcium supplements as your body can only cope with a certain amount of calcium, and if you take too much you may develop kidney stones or other complications.
Your body also needs vitamin D to absorb calcium properly. Vitamin D is produced naturally by your body when your skin is exposed to sunlight and can also be obtained from some foods, such as oily fish. Your doctor may prescribe vitamin D supplements.
Medicines
Your doctor may prescribe the following medicines to increase your bone density.
- Bisphosphonates – these work by slowing down bone loss. Examples include alendronate (eg Fosamax), etidronate (eg Didronel), risedronate (eg Actonel), and zoledronate (eg Aclasta).
- Strontium ranelate (eg Protelos) – this stimulates new bone to grow and reduces bone loss.
- Calcitonin (eg Miacalcic) – this is a hormone usually made by the thyroid gland, it blocks the action of the cells that break down bone.
- Parathyroid hormone peptides (parathyroid hormone (eg Preotact) and teriparatide (eg Forsteo) – these help to regulate calcium levels and the activity of cells involved in bone formation.
- Raloxifene (eg Evista) – this is a synthetic hormone that works by copying the effects of oestrogen on your bones.
- Hormone replacement therapy (HRT) – this relieves symptoms of the menopause by restoring hormones to a pre-menopausal level. HRT has also been shown to reduce osteoporosis, but you probably won’t be prescribed it specifically to treat or prevent the condition.
- Denosumab (Prolia) – given as an injection every six months, it’s a biological treatment that works by blocking the formation of cells that break down bone.
Pain management
Over-the-counter painkillers can help with any pain you have. Always read the patient information leaflet that comes with your medicine. Physiotherapy, hydrotherapy (exercise in water) and TENS (transcutaneous electrical nerve stimulation) and alternative therapies, like acupuncture, may also help. Always ask your doctor or pharmacist for advice before any treatment.
Treatments for men
If your osteoporosis is caused by hypogonadism, your GP may prescribe testosterone replacement therapy.
Some osteoporosis treatments are only licensed for women who have gone through the menopause. However, there are some treatments that are also licensed for men such as the bisphosphonates alendronate (eg Fosamax) and risedronate (eg Actonel) – ask your doctor for advice on which treatments are available and suitable for you.
Prevention of osteoporosis
Changing your lifestyle could help to reduce your chances of developing osteoporosis. A healthy diet [link to healthy eating] and regular exercise [link to physical activity] can increase bone mass, especially in younger people with growing bones.
High-impact exercise, where you support your own weight, is best for strengthening bones. The National Osteoporosis Society recommends jogging, aerobics, tennis, weight-training, dancing and brisk walking. If you aren’t used to exercising, build up your exercise routine gradually. Talk to your GP before you start a new exercise routine if you have any concerns.
Smoking can have a harmful effect on your bone strength and can also cause an early menopause in women. If you smoke, try to give up [link to Giving up smoking]. You should also be careful not to drink too much alcohol [link to sensible drinking].
Adults should aim to have 700mg of calcium every day, which you should be able to get through healthy eating. Also, make sure you get enough vitamin D as this is also important for bone health.
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email.
I think I may be at risk of osteoporosis. Should I have a bone scan?
How much calcium should I be getting to help prevent osteoporosis?
I can’t eat dairy food. How do I make sure I get enough calcium?
My doctor has told me to eat a low-fat diet. How can I get enough calcium if I have to limit cheese and milk?
I have osteoporosis. How do I deal with the pain from broken bones?
My wife has been advised by her GP to eat a calcium-rich diet to reduce her chances of developing osteoporosis. Should I be following this diet too?
Why isn’t spinach a good source of calcium?
I read in the newspaper that calcium supplements can increase the risk of having a heart attack. Should I stop taking them?
I think I may be at risk of osteoporosis. Should I have a bone scan?
Talk to your doctor about what is best for you.
Explanation
Many people don’t know that they have osteoporosis until they break a bone – often a hip, wrist or bones in the spine. However, it’s possible to find out if you have osteoporosis before you have a break using dual X-ray absorptiometry (DEXA or DXA) scanning. DXA scanning is the most common way of diagnosing osteoporosis.
DXA scanning is expensive and its availability may be limited. It is usually only recommended for people at high risk of having osteoporosis. DXA scans to screen for the condition are available from private clinics and hospitals.
If you’re concerned that you’re at risk of osteoporosis, talk to your doctor.
Further information
National Osteoporosis Society
0845 450 0230
www.nos.org.uk
Sources
- Poole KES, Compston JE. Osteoporosis and its management. BMJ 2006; 333:1251–56. www.bmj.com
- Guidelines for the diagnosis and management of osteoporosis in postmenopausal women and men from the age of 50 years in the UK. National Osteoporosis Guideline Group, 2008. www.shef.ac.uk
- Osteoporosis. UK National Screening Committee. www.screening.nhs.uk, accessed 30 May 2010
How much calcium should I be getting to help prevent osteoporosis?
This depends on your age and, if you’re a woman, whether you have been through the menopause.
Explanation
If you think you may be at risk of developing osteoporosis, talk to your GP. If you’re a woman who hasn’t been through the menopause, try to get 700mg of calcium per day. This is the daily amount of calcium recommended for adults by the Food Standards Agency. It should be possible to get 700mg of calcium a day from your diet. If you find this difficult you may need to take a calcium supplement.
Once you reach the menopause, increase the calcium in your diet to 1,000mg a day. This increased level also applies to people diagnosed with osteoporosis. If you’re diagnosed with osteoporosis, you may be given a calcium supplement and your osteoporosis medication.
To give you some idea about how to get enough calcium in your diet, here is the amount of calcium in some everyday foods:
- a 200ml glass of semi-skimmed milk contains 240mg calcium
- a 100g fruit yogurt contains 122mg calcium
- 100g Cheddar cheese contains 739mg calcium
- four slices of white bread contains 175mg calcium
- four slices wholemeal bread contains 105mg calcium
- 100g tinned sardines (in oil) contain 500mg calcium
- 100g tinned salmon contains 91mg calcium
- 100g baked beans contain 53mg calcium
Your body also needs other nutrients to help you absorb calcium, in particular vitamin D. It’s difficult to get enough vitamin D from sunlight and diet alone, particularly if you live in a region that is nearer the North or South Pole than the equator (such as the UK, Canada or southern Argentina), or because you don’t go outside very often. Taking 35 to 50mg of vitamin D a day will reduce your risk of developing osteoporosis as well as various cancers. Talk to your GP or pharmacist before taking vitamin D supplements, and always read the patient information leaflet that comes with your supplements.
Further information
Food Standards Agency
www.eatwell.gov.uk
National Osteoporosis Society
0845 450 0230
www.nos.org.uk
Sources
- Guidelines for the diagnosis and management of osteoporosis in postmenopausal women and men from the age of 50 years in the UK. National Osteoporosis Guideline Group, 2008. www.shef.ac.uk
- Calcium. Food Standards Agency. www.eatwell.gov.uk, accessed 12 May 2010
- Healthy bones – facts about food. National Osteoporosis Society. www.nos.org.uk, accessed 12 May 2010
- Bischoff-Ferrari HA, Giovannucci E, Willett WC, et al. Estimation of optimal serum concentrations of 25-hydroxyvitamin d for multiple health outcomes. Am J Clin Nutr 2006; 84:18–28. www.ajcn.org
- Pearce SHS, Cheetham TD. Diagnosis and management of vitamin d deficiency. BMJ 2010; 340:b5664. www.bmj.com
- Update on vitamin D position statement by the scientific advisory committee on nutrition. Scientific Advisory Committee on Nutrition. www.sacn.gov.uk, accessed 10 May 2010
- Drug treatment. National Osteoporosis Society. www.nos.org.uk, accessed 12 May 2010
- Vitamin D. British National Formulary. www.bnf.org, accessed 12 May 2010
- Management of osteoporosis. Scottish Intercollegiate Guidelines Network (SIGN), 2004. Guidance 71. www.sign.ac.uk
I can’t eat dairy food. How do I make sure I get enough calcium?
It should still be possible to get enough calcium in your diet.
Explanation
Even if you don’t eat milk or dairy food there are other options. Good sources of calcium include canned sardines, soya beans and tofu, bread, pulses, green vegetables, dried fruit (especially figs), nuts and seeds (particularly almonds and sesame seeds). If you use soya, rice or oat milk, choose one with added calcium.
If you’re concerned about how much calcium you’re getting from your diet, talk to your GP or a dietician.
Further information
Food Standards Agency
www.eatwell.gov.uk
National Osteoporosis Society
0845 450 0230
www.nos.org.uk
Sources
- Calcium. Food Standards Agency. www.eatwell.gov.uk, accessed 12 May 2010
- Healthy bones – facts about food. National Osteoporosis Society. www.nos.org.uk, accessed 12 May 2010
My doctor has told me to eat a low-fat diet. How can I get enough calcium if I have to limit cheese and milk?
It’s best to eat some dairy foods each day as they are good sources of calcium. There are many low-fat dairy products available.
Explanation
You can either try switching to lower fat options or try using a little less high-fat foods such as hard cheese. Try switching from:
- whole milk to semi-skimmed or skimmed milk
- Cheddar or Edam cheese to cottage cheese
- cream to yogurt or low-fat crème fraîche in cooking or with desserts
- butter to low-fat spread
Further information
- Food Standards Agency
Source
- Milk and dairy. Food Standards Agency. www.eatwell.gov.uk, accessed 30 May 2010
I have osteoporosis. How do I deal with the pain from broken bones?
Talk to your GP. It’s important to explore all the options until you find something that helps you.
Explanation
If you break a bone, you will feel immediate pain that can last until the bone and surrounding tissue heals. Everyone’s experience of fractures is different. However, vertebral (spine) fractures in particular can cause severe pain. If you go into hospital after a break, your doctors will try and get the best possible pain relief for you.
You can also have longer-term, chronic pain even after your bone has healed. This can happen if your posture changes after a fracture. This can put a strain on your surrounding ligaments and muscles. Ongoing pain after a fracture can affect your quality of life.
It’s important that your doctor helps you to find an approach that works for you. There are different options available. Your doctor is likely to suggest trying either over-the-counter or stronger prescription painkillers. If these don't give you enough pain relief, talk to your doctor about what else you can try – this may include some the following options.
- Calcitonin – a medicine that is usually prescribed by hospitals rather than by your GP. It has been shown to help acute and chronic pain due to a fracture of the spine.
- Acupuncture or TENS (transcutaneous electrical nerve stimulation). TENS involves using tiny electrical pulses to block pain. Both acupuncture and TENS can give pain relief for some people and are worth trying.
- Physical exercises that strengthen your back (physiotherapy).
- Hydrotherapy (exercise and physiotherapy treatment based in a pool).
- Your doctor may be able to refer you to a specialist pain clinic.
- Self-management courses can help you to cope with long-term pain. Various organisations run these courses – ask your doctor for information about courses in your area.
If the pain is severe enough to make you depressed, talk to your doctor about some form of talking (psychological) therapy. Some people may also be offered antidepressant medicines. In low doses, antidepressants can help control nerve pain.
Further information
- National Osteoporosis Society
0845 450 0230
www.nos.org.uk
- The British Pain Society
Sources
- Living with osteoporosis and broken bones. National Osteoporosis Society. www.nos.org.uk, accessed 12 May 2010
- Management of osteoporosis. Scottish Intercollegiate Guidelines Network (SIGN), 2004. Guidance 71. www.sign.ac.uk
- Living with broken bones – making life easier after fracture. National Osteoporosis Society. www.nos.org.uk, accessed 30 May 2010
My wife has been advised by her GP to eat a calcium-rich diet to reduce her chances of developing osteoporosis. Should I be following this diet too?
Osteoporosis doesn’t only affect women, men can get it too. If you join your wife in eating a well-balanced diet that includes a lot of calcium-rich foods, it should help you build and maintain strong bones. This in turn will help prevent you from developing osteoporosis.
Explanation
Osteoporosis is often associated with women because it affects more women than men. Although osteoporosis affects half of all women over the age of 50, it also affects one in five men over 50, putting them at increased risk of fractures too.
If you eat a well-balanced diet that includes foods that are rich in calcium, it will help you build and maintain strong bones, which in turn will help prevent osteoporosis. Good sources of calcium include:
- milk and dairy products
- canned fish with bones
- fortified breakfast cereal
- soya bean products
- green leafy vegetables (except for spinach)
- dried fruit
Your body needs vitamin D to help absorb calcium. The best source of vitamin D is exposure to sunlight. You can also get vitamin D from foods such as oily fish, eggs and margarine and from supplements.
Weight-bearing exercise is also important to build healthy bones. Weight-bearing exercises are ones that mean your body carries its own weight, such as walking (but not swimming). Other examples include jogging, dancing, tennis, volleyball and netball.
If you or your wife is at increased risk of developing osteoporosis, your GP may recommend calcium and vitamin D supplements. Always read the information leaflet that comes with your supplements and if you have any questions, ask your pharmacist for advice.
Further information
- National Osteoporosis Society
0845 450 0230
www.nos.org.uk
Sources
- About osteoporosis. National Osteoporosis Society. www.nos.org.uk, accessed 12 May 2010
- Poole KES, Compston JE. Osteoporosis and its management. BMJ 2006; 333:1251–56. www.bmj.com
- Calcium. Food Standards Agency. www.eatwell.gov.uk, accessed 12 May 2010
- Healthy bones – facts about food. National Osteoporosis Society. www.nos.org.uk, accessed 12 May 2010
- Vitamin D. Food Standards Agency. www.eatwell.gov.uk, accessed 30 May 2010
- Exercise for osteoporosis and falls prevention. Osteoporosis Australia. www.osteoporosis.org.au, accessed 30 May 2010
Why isn’t spinach a good source of calcium?
Although spinach has a high calcium content compared with other foods, the calcium is bound to a substance called oxalate, which means that your body can’t absorb it. So, although spinach is a good source of other vitamins and minerals it isn't a good source of calcium.
Explanation
The calcium content of spinach is quite high compared with other foods. For example, 100g of boiled spinach contains around 160mg of calcium compared with 75mg in the same amount of spring greens. But spinach isn’t recommended as a calcium-rich source of food because the calcium is bound to a substance called oxalate, which stops your body from absorbing it.
If you’re trying to increase the amount of calcium in your diet, you should eat other calcium-rich foods such as:
- milk and dairy products
- canned fish with bones
- fortified breakfast cereal
- soya bean products
- other green leafy vegetables
- dried fruit
Your body also needs vitamin D to help absorb the calcium from food. The best source of vitamin D is exposure to sunlight, but you can also get it from foods such as oily fish, eggs and margarine and from supplements.
Further information
- Food Standards Agency
- National Osteoporosis Society
0845 450 0230
www.nos.org.uk
Sources
- Calcium. Food Standards Agency. www.eatwell.gov.uk, accessed 12 May 2010
- Healthy bones – facts about food. National Osteoporosis Society. www.nos.org.uk, accessed 12 May 2010
- Vitamin D. Food Standards Agency. www.eatwell.gov.uk, accessed 30 May 2010
I read in the newspaper that calcium supplements can increase the risk of having a heart attack. Should I stop taking them?
There is some evidence that calcium supplements increase the risk of heart attacks in women who have gone through the menopause. However, as other studies have reported other findings, more research is needed in this area before conclusions can be drawn. If your GP has recommended that you take calcium supplements because you’re at risk of osteoporosis, you should talk to him or her before stopping them.
Explanation
Calcium supplements are sometimes advised for women who have gone through the menopause to keep their bones healthy. A recent study, however, found that heart attacks were more common in women taking calcium supplements than in women taking a placebo (dummy pills). Scientists don’t yet know why calcium supplements could cause this effect, but high calcium levels could lead to a build-up of calcium in the blood vessels. More research is needed to understand the link between calcium supplements and heart attacks.
If your GP has recommended that you take calcium supplements, it may be because he or she thinks that you’re at risk of osteoporosis. In the UK, the recommended calcium intake is 700mg a day for adults and up to 1,200mg if you have been diagnosed with osteoporosis and are on prescribed drug treatments. If you get adequate calcium from your diet, you may not need calcium supplements.
You should always talk to your GP before stopping any medicine or supplement that has been recommended for you. It’s important to remember that any risks associated with taking calcium supplements must be balanced against the risk of osteoporosis and fractures that may happen if you don’t take your calcium supplements.
Further information
- National Osteoporosis Society
0845 450 0230
www.nos.org.uk
Sources
- Calcium. Food Standards Agency. www.eatwell.gov.uk, accessed 12 May 2010
- Bolland MJ, Barber PA, Doughty RN, et al. Vascular events in healthy older women receiving calcium supplementation: Randomised controlled trial. BMJ 2008; 336: 262–66. www.bmj.com
- Drug treatments for osteoporosis. National Osteoporosis Society. www.nos.org.uk, accessed 30 May 2010
- Personal communication, Mr Roger M Tillman, MB, ChB FRCS, FRCS Orth. Consultant Orthopaedic Surgeon, Royal Orthopaedic Hospital, Birmingham, 16 June 2010
Related topics
- DEXA scan
- Healthy eating
- Menopause
- Physical activity
- Skin cancer
- Sun care
Further information
National Osteoporosis Society
0845 450 0230
www.nos.org.uk
Sources
- Alendronate, etidronate, risedronate, raloxifene and strontium ranelate for the primary prevention of osteoporotic fragility fractures in postmenopausal women (amended). National Institute for Health and Clinical Excellence (NICE), January 2010. Technology Appraisal Guidance 160. www.nice.org.uk
- About osteoporosis. National Osteoporosis Society. www.nos.org.uk, accessed 12 May 2010
- Poole KES, Compston JE. Osteoporosis and its management. BMJ 2006; 333:1251–56 www.bmj.com
- Who is at risk of osteoporosis and broken bones?. National Osteoporosis Society. www.nos.org.uk, accessed 12 May 2010
- Osteoporosis. Health Evidence Bulletins Wales. www.hebw.cf.ac.uk, accessed 12 May 2010
- Guidelines for the diagnosis and management of osteoporosis in postmenopausal women and men from the age of 50 years in the UK. National Osteoporosis Guideline Group, 2008. www.shef.ac.uk
- Scans and tests and osteoporosis. National Osteoporosis Society. www.nos.org.uk, accessed 12 May 2010
- Guidelines for the promotion of physical activity with older people. British Heart Foundation National Centre for Physical Activity and Health, 2008. www.bhfactive.org.uk
- Calcium. Food Standards Agency. www.eatwell.gov.uk, accessed 12 May 2010
- Healthy bones – facts about food. National Osteoporosis Society. www.nos.org.uk, accessed 12 May 2010
- Bischoff-Ferrari HA, Giovannucci E, Willett WC, et al. Estimation of optimal serum concentrations of 25-hydroxyvitamin d for multiple health outcomes. Am J Clin Nutr 2006; 84:18–28. www.ajcn.org
- Pearce SHS, Cheetham TD. Diagnosis and management of vitamin D deficiency. BMJ 2010; 340:b5664. www.bmj.com
- Update on vitamin D position statement by the scientific advisory committee on nutrition. Scientific Advisory Committee on Nutrition. www.sacn.gov.uk, accessed 10 May 2010
- Drug treatment. National Osteoporosis Society. www.nos.org.uk, accessed 12 May 2010
- Osteoporosis. British National Formulary. www.bnf.org, accessed 12 May 2010
- New osteoporosis treatment denosumab (prolia) launched in the UK. National Electronic Library for Medicines (NELM). www.nelm.nhs.uk, accessed 31 May 2010
- Living with osteoporosis and broken bones. National Osteoporosis Society. www.nos.org.uk, accessed 12 May 2010
- Alendronic acid. British National Formulary. www.bnf.org, accessed 12 May 2010
- What is osteoporosis?. National Osteoporosis Society. www.nos.org.uk, accessed 12 May 2010
- Healthy bones. National Osteoporosis Society. www.nos.org.uk, accessed 12 May 2010
- Bradbury J. Mechanism found for smoking-induced early menopause. The Lancet 2001; 358(9277):215. www.thelancet.com
- Vitamin D. British National Formulary. www.bnf.org, accessed 12 May 2010
- Osteoporosis. UK National Screening Committee. www.screening.nhs.uk, accessed 30 May 2010
- Management of osteoporosis. Scottish Intercollegiate Guidelines Network (SIGN), 2004. Guidance 71. www.sign.ac.uk
- Milk and dairy. Food Standards Agency. www.eatwell.gov.uk, accessed 30 May 2010
- Living with broken bones – making life easier after fracture. National Osteoporosis Society. www.nos.org.uk, accessed 30 May 2010
- Vitamin D. Food Standards Agency. www.eatwell.gov.uk, accessed 30 May 2010
- Exercise for osteoporosis and falls prevention. Osteoporosis Australia. www.osteoporosis.org.au, accessed 30 May 2010
- Bolland MJ, Barber PA, Doughty RN, et al. Vascular events in healthy older women receiving calcium supplementation: randomised controlled trial. BMJ 2008; 336: 262–66. www.bmj.com
- Drug treatments for osteoporosis. National Osteoporosis Society. www.nos.org.uk, accessed 30 May 2010
- Personal communication, Mr Roger M Tillman, MB, ChB FRCS, FRCS Orth. Consultant Orthopaedic Surgeon, Royal Orthopaedic Hospital, Birmingham, 16 June 2010
















