Rheumatoid arthritis
This factsheet is for people who have rheumatoid arthritis, or who would like information about it.
Rheumatoid arthritis (RA) occurs as a result of the immune system causing inflammation of the lining of joints and surrounding structures.
About rheumatoid arthritis
Symptoms of rheumatoid arthritis
Causes of rheumatoid arthritis
Diagnosis of rheumatoid arthritis
Treatment of rheumatoid arthritis
Living with rheumatoid arthritis
About rheumatoid arthritis
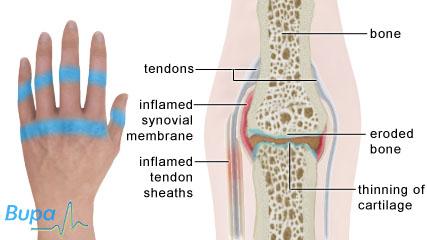
Arthritis means inflammation of the joints. Rheumatoid arthritis (RA) is an autoimmune disease. This means that the white cells and antibody proteins in your blood that usually fight infections enter your joints and cause inflammation. This causes heat, swelling and excess fluid to be produced.
Eventually, this may lead to thinning of the cartilage that covers the ends of your bones, and may cause the bone to be worn away. RA may also cause inflammation of the sheaths around your tendons. Rarely, the condition can affect other parts of your body, such as your lungs.
RA affects more than 350,000 people in the UK and can start at any age.
Symptoms of rheumatoid arthritis
You may notice discomfort initially in a few joints such as your fingers, knuckles, wrists or the balls of your feet. Typically RA is a ‘symmetrical’ arthritis – this means it affects both wrists or both hands in the same way. For most people, RA develops quite slowly at first. Other people find the condition comes on quickly and painfully, making it difficult to carry out daily activities. Symptoms include:
- pain and swelling around the joint, making it tender and warm
- stiffness in the morning, or if you sit for a long time
- poor grip strength
- tiredness, making you feel irritable and depressed
- flu-like symptoms such as fever
- weight loss
- rheumatoid nodules – fleshy lumps that usually appear on your hands, feet and elbows
RA affects everyone differently. You may find that your symptoms come and go with little pain, swelling or inflammation in between the flare-ups. Flare-ups can last for a few days to a couple of months. You probably won’t be able to predict when they will occur.
Causes of rheumatoid arthritis
The exact reasons why you may develop RA aren’t fully understood at present. There are a number of things that seem to be involved. Women are nearly three times more likely to get RA than men. Symptoms tend to improve during pregnancy, suggesting that hormones and the immune system may be involved.
It’s possible that RA is triggered by an infection or virus, but there isn’t any evidence to prove this.
Having certain genes makes it more likely that you will get RA, and the disease runs in some families.
Lifestyle factors may also increase your risk, for example, if you smoke or are obese.
Diagnosis of rheumatoid arthritis
If you think you may you have RA, even if your symptoms are mild, see your GP. It’s important to be referred to a specialist to start treatment as early as possible, especially if you have had symptoms for more than three months. Treatment focuses on reducing inflammation to limit the damage to your joints. If left untreated, RA may lead to serious disability.
Your GP will ask about your symptoms and examine you. He or she may also ask you about your medical history. There’s no single test that can diagnose RA but your GP may refer you for one or more of the following.
- A blood test for a marker called rheumatoid factor, present in eight in 10 people with RA.
- Anti-CCP antibody testing.
- Blood tests for anaemia (a condition when you have too few red blood cells or not enough haemoglobin in your blood) – eight in 10 people with RA have anaemia.
- X-ray, ultrasound or magnetic resonance imaging (MRI) to look for changes in your joints.
Treatment of rheumatoid arthritis
Self-help
There are things you can do to help ease the symptoms of RA.
- Find a balance between exercise and rest. It’s important to exercise to stop your joints from becoming weak and stiff but don’t do too much. Swimming is excellent because it strengthens your muscles and joints without putting any strain on them. A physiotherapist can tailor a programme to suit you.
- Losing excess weight will reduce the pressure on your joints.
- An occupational therapist can suggest ways of making everyday tasks easier and may be able to provide you with specialist equipment.
- Eat a healthy, balanced diet and cut down on saturated fats.
- Use a splint on the affected joint and rest it during a flare-up.
There is limited evidence that taking certain food supplements can help RA. These include:
- omega-3 fatty acids – found in oily fish such as mackerel, salmon and sardines, and some plant seed oils and nuts
- borage seed oil
- evening primrose oil
Speak to your GP if you’re thinking of taking any supplements.
Medicines
No medicine can cure RA, but there are many that can help symptoms.
- Painkillers such as paracetamol may help to relieve pain and stiffness.
- Non-steroidal anti-inflammatory drugs (NSAIDs) reduce symptoms of inflammation, relieving pain and swelling.
- Disease-modifying anti-rheumatic drugs (DMARDs) slow down the progression of RA and ease its symptoms. They can take several months to work so it’s important to continue taking them. You may need to try one or more.
- Biological medicines made from animal or human proteins block the progress of RA in your immune system. You may be eligible to try these if other medicines haven’t helped your symptoms.
Always ask your doctor for advice and read the patient information leaflet that comes with your medicine.
Non-surgical treatments
NSAIDs are available as creams or gels that you can rub onto painful areas. They aren’t usually sufficient for treating inflamed joints.
If you have a bad flare-up, you may be offered a corticosteroid injection into a specific joint to reduce inflammation.
Surgery
As medical treatments have improved it’s now less likely that you will need surgery to treat RA. However, if you have severely damaged joints and medicines haven’t helped, your doctor may recommend one of the following operations to reduce pain and discomfort.
- A hip or knee replacement.
- Synovectomy to remove the lining of an inflamed joint.
- Removal or repair of severely inflamed tendons.
- Surgery to fuse a joint to make it more stable.
Complementary therapies
Complementary therapies such as acupuncture and aromatherapy may relieve pain and make you feel more relaxed. However, they have no effect on how fast the disease progresses. Speak to your doctor before trying any complementary therapy as it may affect conventional medicines.
Living with rheumatoid arthritis
You may find RA upsetting and frustrating at times. It’s important to tell your doctor how it’s affecting your life so you get the most suitable treatment. You may need to make changes to your daily life but there are people who can help to make this easier.
There is some evidence to suggest that if you have an inflammatory condition such as rheumatoid arthritis, you may be at a greater risk of heart disease. Therefore, it’s important to take steps to minimise your risk of developing this, for example by reducing the amount of saturated fat in your diet and taking regular exercise. Your GP can give you more advice and information.
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email.
If I have rheumatoid arthritis (RA), should I see an occupational therapist?
Will rheumatoid arthritis (RA) affect my whole body?
Will exercise make my rheumatoid arthritis (RA) worse?
If I have rheumatoid arthritis (RA), should I see an occupational therapist?
Answer
Yes, an occupational therapist can be very helpful, especially if you’re having problems with everyday activities.
Explanation
Occupational therapists are health professionals who can give practical assistance to help you manage everyday tasks and increase your independence. Under the NHS and Community Care Act 1990, you’re entitled to a needs assessment from social services.
An occupational therapist will assess your condition before looking at your needs at home or with transport, hobbies and work. He or she will then offer practical advice on:
- repositioning yourself during activities such as cooking
- getting enough rest
- protecting your joints
- gadgets and home and work adaptations (including adaptations for cars) – local Disabled Living Centres offer the chance to try gadgets and you can also get advice from Mobility Centres
- splints to ease the strain and pain on hand and wrist joints while carrying out activities, and to keep your joints stable while resting
Further information
Arthritis Care
0808 800 4050
www.arthritiscare.org.uk
Arthritis Research Campaign
0870 850 5000
www.arc.org.uk
Disabled Living Centres
0870 770 2866
www.assist-uk.org
The Forum of Mobility Centres
0800 559 3636
www.mobility-centres.org.uk
Ricability
020 7427 2460
www.ricability.org.uk
Sources
Occupational therapy and arthritis. Arthritis Research Campaign. www.arc.org.uk, accessed 7 July 2009
Occupational therapy. Arthritis Care. www.arthritiscare.org.uk, accessed 7 July 2009
In the home. Arthritis Care. www.arthritiscare.org.uk, accessed 7 July 2009
Will rheumatoid arthritis (RA) affect my whole body?
Answer
It's difficult to say as RA affects everyone differently.
Explanation
Once it progresses, RA can spread to other joints. However, there are many effective therapies that can reduce its effect.
More rarely, inflammation can affect your eyes, making them dry and irritated, and your tear glands, salivary glands, blood vessels, lungs and even your heart.
Most people with RA have other general problems such as stiffness, tiredness and feeling unwell. However, medicines will help to control your RA. Your physiotherapist and occupational therapist can also give you advice on making lifestyle changes to ease symptoms.
Further information
Arthritis Care
0808 800 4050
www.arthritiscare.org.uk
Arthritis Research Campaign
0870 850 5000
www.arc.org.uk
Sources
Rheumatoid arthritis. Arthritis Research Campaign. www.arc.org.uk, accessed 7 July 2009
Rheumatoid arthritis. Arthritis Care. www.arthritiscare.org.uk , accessed 7 July 2009
Will exercise make my rheumatoid arthritis (RA) worse?
Answer
Not if you exercise with care. There are proven benefits from exercise if you have RA. The key is getting a balance between rest and exercise.
H3 Explanation
Inflamed joints benefit from rest but if you don't keep them moving, they will stiffen and your muscles will weaken.
Get advice specifically designed for you – a physiotherapist can help with this. However, don’t do contact and vigorous sports, such as football and squash. Swimming is by far the best form of exercise as the water supports your weight.
An exercise programme should include the following.
- Strengthening exercises to target the muscles around your affected joints and improve your stability and mobility, reducing pain and disability.
- Range of movement exercises to keep you flexible and moving around – doing these in the morning can help ease stiffness, and before going to bed can help to prevent it.
- Aerobic exercise that increases your heart rate and makes you slightly out of breath – this helps reduce pain and improves your health. Walking, yoga and cycling or everyday activities such as housework or gardening can help.
Some tips that may help you when exercising include the following.
- Make it part of your daily routine and build up slowly.
- Have a warm bath or shower, or place a hot water bottle on affected joints before exercising.
- Never force a painful joint. It’s common to feel some pain as you build up your exercise programme. However, if any pain lasts longer than two hours after exercising, contact your GP.
- Always wear cushioned and supportive footwear.
Further information
Arthritis Care
0808 800 4050
www.arthritiscare.org.uk
Arthritis Research Campaign
0870 850 5000
www.arc.org.uk
Sources
Rheumatoid arthritis. Arthritis Research Campaign. www.arc.org.uk, accessed 7 July 2009
Keeping active. Arthritis Care. www.arthritiscare.org.uk, accessed 7 July 2009
Exercise and arthritis. Arthritis Care.www.arthritiscare.org.uk, accessed 7 July 2009
Related topics
Anaemia – a general overview
NSAIDs
Osteoarthritis
Psoriatic arthritis
Further information
Arthritis Care
0808 800 4050
www.arthritiscare.org.uk
Arthritis Research Campaign
0870 850 5000
www.arc.org.uk
Sources
- Introducing arthritis. Arthritis Research Campaign. www.arc.org.uk, accessed 6 July 2009
- Rheumatoid arthritis. Arthritis Research Campaign. www.arc.org.uk, accessed 6 July 2009
- Rheumatoid arthritis. Arthritis Care. www.arthritiscare.org.uk, accessed 6 July 2009
- Simon C, Everitt H, Kendrick T. Oxford handbook of general practice. 2nd ed. Oxford: Oxford University Press, 2006
- Niewold TB, Harrison MJ, Paget SA. Anti-CCP antibody testing as a diagnostic and prognostic tool in rheumatoid arthritis. QJM 2007; 100(4):193–201. doi:10.1093/qjmed/hcm015
- Rheumatoid arthritis. National clinical guideline for management and treatment in adults. National Institute for Health and Clinical Excellence (NICE), 2009. www.nice.org.uk
- Rheumatoid arthritis. Clinical Knowledge Summaries. www.cks.library.nhs.uk, accessed 6 July 2009
- Looking after your joints when you have rheumatoid arthritis. Arthritis Research Campaign. www.arc.org.uk, accessed 7 July 2009
- Occupational therapy and arthritis. Arthritis Research Campaign. www.arc.org.uk, accessed 7 July 2009
- Diet and arthritis. Arthritis Research Campaign. www.arc.org.uk, accessed 7 July 2009
- Drugs and arthritis (general information). Arthritis Research Campaign. www.arc.org.uk, accessed 7 July 2009
- Henry JA. The British Medical Association new guide to medicines and drugs. 6th ed. London: Dorling Kindersley, 2004
- Scott DL, Shipley M, Dawson A, et al. The clinical management of rheumatoid arthritis and osteoarthritis: strategies for improving clinical effectiveness. Rheumatology 1998; 37:546–54. doi:10.1093/rheumatology/37.5.546
- Complementary therapy. Arthritis Care. www.arthritiscare.org.uk, accessed 7 July 2009
- Surgery. Arthritis Care. www.arthritiscare.org.uk, accessed 7 July 2009
- Quyyumi AA. Inflamed joints and stiff arteries. Is rheumatoid arthritis a cardiovascular risk factor? Circulation 2006; 114:1137–39. doi:10.1161/CIRCULATIONAHA.106.648139
- Luqmani R, Hennell S, Estrach C, et al. British Society for Rheumatology and British Health Professionals in Rheumatology guideline for the management of rheumatoid arthritis (after the first 2 years). Rheumatology 2009; 48(4):436–39. doi:10.1093/rheumatology/ken450b
- Complementary and alternative medicines for the treatment of rheumatoid arthritis, osteoarthritis and fibromyalgia. Arthritis Research Campaign, 2009. www.arc.org.uk