Wisdom teeth removal
This factsheet is for people who are having their wisdom teeth removed, or who would like information about it.
Wisdom teeth removal involves taking out the wisdom teeth at the back of the mouth that are causing problems.
You will meet the dentist or oral surgeon carrying out your procedure to discuss your care. It may differ from what is described here as it will be designed to meet your individual needs.
About wisdom teeth removal
What are the alternatives?
Preparing for wisdom teeth removal
What happens during wisdom teeth removal
What happens afterwards
Recovering from wisdom teeth removal
What are the risks?
About wisdom teeth removal
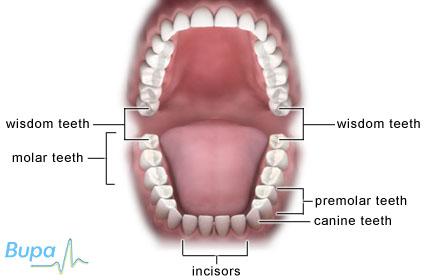
Wisdom teeth usually emerge from your gums between the ages of 17 and 24. They are the last of the large grinding teeth at the back of your mouth (molars). Some people never develop wisdom teeth but you could have up to four – one in each corner of your mouth.
For most people, wisdom teeth don't cause any problems so don't need to be removed. However, if there isn't enough space for them to grow at the back of your mouth they become what is known as impacted wisdom teeth, and can cause pain, swelling and/or infection.
Having your impacted wisdom teeth surgically removed (extracted) can relieve your symptoms. It may be possible for your dentist to remove your wisdom teeth, or he or she may refer you to an oral surgeon.
What are the alternatives?
Antibiotics can help treat an infection, but your symptoms may flare up again. Having your wisdom teeth removed is often the only way to permanently relieve your symptoms.
Preparing for wisdom teeth removal
Your dentist or oral surgeon will explain how to prepare for your procedure. For example, if you smoke, you may be asked to stop as smoking increases your risk of getting a wound infection, which can slow your recovery.
The operation is usually done under local anaesthesia. This completely blocks pain from your gums and you will stay awake during the procedure. You may be offered a sedative to help you relax during the operation. If you go to a hospital and your wisdom teeth are particularly challenging to remove, you may be given general anaesthesia. This means you will be asleep during the procedure. Your dentist or oral surgeon will let you know which type of anaesthesia is most suitable for you.
If you're having a general anaesthetic, you will be asked to follow fasting instructions. This means not eating or drinking, typically for about six hours beforehand. However, it’s important to follow your dentist or oral surgeon’s advice.
Your dentist or oral surgeon will discuss with you what will happen before, during and after your procedure, and any pain you might have. This is your opportunity to understand what will happen, and you can help yourself by preparing questions to ask about the risks, benefits and any alternatives to the procedure. This will help you to be informed, so you can give your consent for the procedure to go ahead, which you may be asked to do by signing a consent form.
What happens during wisdom teeth removal
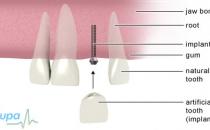
The procedure for removing your wisdom teeth will depend how deeply impacted your teeth are. Many wisdom teeth can be extracted simply like any other molar. Once the anaesthetic has taken effect, your dentist or oral surgeon will widen the socket (the area your tooth sits in) using a tool called an elevator or a pair of special forceps. He or she will then move the tooth from side to side until it is loose enough to be removed completely.
However, if your tooth is more difficult to remove, your dentist or oral surgeon will cut through your gums and may remove some of your jawbone to reach your tooth. He or she will remove your wisdom teeth and then close your wounds with stitches if necessary.
Most wisdom teeth only take a few minutes to remove, but the more difficult cases can take around 20 minutes.
What to expect afterwards
You will need to rest until the effects of the general anaesthetic or sedation have passed.
After a local anaesthetic, it may be several hours before the feeling comes back into your jaw. Take special care not to chew on the area or have any food or drinks that are too hot, as these could burn the area.
You will be able to go home when you feel ready.
If you had a general anaesthetic or sedation you will need to arrange for someone to drive you home. You should try to have a friend or relative stay with you for the first 24 hours.
Your dentist or oral surgeon will give you some advice about looking after your teeth and gums before you go home. You may be given painkillers, antibiotics and mouthwash solutions to take home. You may also be given a date for a follow-up appointment.
Dissolvable stitches will disappear on their own in seven to 10 days. Non-dissolvable stitches are removed a week after surgery.
Recovering from wisdom teeth removal
If you need them, you can take over-the-counter painkillers such as paracetamol or ibuprofen. Follow the instructions in the patient information leaflet that comes with your medicine and ask your pharmacist for advice. Don’t take aspirin because this can make bleeding worse.
Don't vigorously rinse out your mouth during the first 24 hours after having a wisdom tooth removed because this can disturb blood clots that help the healing process. After meals, you can rinse gently with warm salt water (half a teaspoon of table salt dissolved in a glass of water).
You should brush your teeth as usual, but keep your toothbrush away from the healing wound for the first couple of days.
At first, you may feel small fragments of bone with your tongue. These are the edges of the tooth socket and will soon disappear as your gum heals.
Eating and drinking
To begin with, you should eat soft foods, gradually returning to your usual diet once your jaw feels less stiff.
Bleeding
If your gum bleeds, fold a clean handkerchief or piece of gauze, place it on your bleeding gum and bite on it for at least 10 to 15 minutes. Don't rinse your mouth out or lie down until the bleeding has stopped.
Most people don't experience any problems after having their wisdom teeth removed. However, contact your dentist or your GP immediately if you develop any of the following symptoms:
- bleeding that doesn't stop after applying pressure, or that lasts for more than half an hour
- difficulty in breathing or swallowing
- severe pain that isn't helped by painkillers
- a high temperature
- swelling that continues for more than three days after your operation
What are the risks?
Wisdom teeth removal is commonly performed and generally safe. However, in order to make an informed decision and give your consent, you need to be aware of the possible side-effects and the risk of complications of this procedure.
Side-effects
These are the unwanted, but mostly temporary effects of a successful treatment, for example feeling sick as a result of a general anaesthetic.
You may have some facial swelling, bruising, pain or jaw stiffness for up to two weeks. These symptoms are usually at their worst for the first two or three days and then gradually improve.
Complications
This is when problems occur during or after the operation. Most people aren’t affected. The possible complications of any operation include an unexpected reaction to the anaesthetic or excessive bleeding.
Specific complications to having your wisdom teeth extracted are uncommon but may include:
- infection
- accidental damage to other teeth and your jaw during your operation
- severe pain caused by dry socket – this is when the blood clot breaks away from the wound exposing the bone and nerves, causing pain and delaying healing
- numbness in your lower lip or tongue, or changes to taste – this can be caused by nerve damage and there is a small chance that this could be permanent
- jaw stiffness – it's possible that you may not be able to open your mouth fully
The exact risks are specific to you and will differ for every person, so we have not included statistics here. Ask your dentist or oral surgeon to explain how these risks apply to you.
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email.
My dentist told me to use a mouthwash after eating – why is this?
What is dry socket?
My wisdom teeth are causing me a lot of pain and I'm pregnant. Is it safe to have them taken them out?
My dentist told me to use a mouthwash after eating – why is this?
Brushing your teeth after having your wisdom teeth removed can be difficult or uncomfortable. Your dentist or oral surgeon will give you advice on using mouthwashes and how to prepare a salt water mouthwash to keep your wounds clean.
Explanation
If you can, try to brush your teeth as usual but you may find that it's too sore to clean the teeth near your wounds. If this is the case, you can use mouthwashes.
Mouthwashes help to remove food debris and can help to soothe your wounds and prevent infection.
You can make a salt water mouthwash by dissolving half a teaspoon of salt in a cup of warm water. Don't use very hot or cold water as this can make your wounds bleed.
Alternatively you can use a chlorhexidine mouthwash, which you can buy over the counter. Chlorhexidine is an antiseptic that also prevents plaque. Chlorhexidine can also reduce the chances of you developing dry socket - a condition caused by the breakdown or loss of the blood clot that forms in your tooth socket after you have had a tooth removed.
Further information
-
British Dental Health Foundation
0845 063 1188
www.dentalhealth.org.uk
Sources
- Removal of impacted wisdom teeth. British Association of Oral and Maxillofacial Surgeons. www.baoms.org.uk, published March 2007
- Treatments: Tooth extraction. British Dental Association. www.bdasmile.org, accessed 22 June 2010
- Joint Formulary Committee, British National Formulary. 57th ed. London: British medial Association and Royal Pharmaceutical Society of Great Britain, 2009:612
What is dry socket?
Dry socket (alveolar osteitis) is a condition caused by the breakdown or loss of the blood clot that forms in your tooth socket after you have had a tooth removed. The blood clot protects your socket and helps your wound to heal.
Explanation
Dry socket can cause severe pain that isn't relieved by painkillers. Loss of the blood clot from the tooth socket can lead to infection, nerve irritation and delays to your healing.
Pain from dry socket usually begins about three to five days after having your wisdom teeth removed. If you think you have dry socket, you should visit your dentist immediately.
Your dentist will rinse out your empty socket and may then pack the socket with a dressing soaked in painkillers and antiseptics.
You may also be prescribed a course of antibiotics to prevent the socket from becoming infected. Always ask your dentist for advice and read the patient information leaflet that comes with your medicine.
After treatment for dry socket you should rest and it will usually heal within about 10 days.
Further information
-
British Dental Health Foundation
0845 063 1188
www.dentalhealth.org.uk
Sources
- Treatments: Tooth extraction. British Dental Association. www.bdasmile.org, accessed 22 June 2010
- Cowan P. Treatment of third molar teeth – surgery. J Ir Dent Assoc, 2006. 52(1):7. www.dentist.ie
- Management of unerupted and impacted third molar teeth. Scottish Intercollegiate Guidelines Network (SIGN), 2000, SIGN Publication number 43. www.sign.ac.uk
My wisdom teeth are causing me a lot of pain and I'm pregnant. Is it safe to have them taken them out?
Yes. Wisdom teeth removal is perfectly safe if you're pregnant. Your dentist or oral surgeon will discuss your options with you.
Explanation
If you're pregnant, or think you might be, let your dentist or oral surgeon know. Essential dental treatment is safe for pregnant women, but some parts of the treatment may be changed to suit you.
Although the X-ray images you need before your teeth are removed are probably safe as the beam of X-rays doesn't go near your developing baby, it’s generally best to avoid X-rays while you’re pregnant, unless they are essential.
If you do need to have your wisdom teeth removed, your dentist or oral surgeon will probably recommend local anaesthesia, which can be used safely in pregnancy. A local anaesthetic completely blocks feeling from the area and you will stay awake during the procedure. It may be possible for you to have general anaesthesia if you need to – for example, if your teeth will be difficult to extract. A general anaesthetic means you will be asleep during the procedure. However, a general anaesthetic can affect your baby.
If you need to take painkillers after your wisdom teeth have been taken out, you can take paracetamol. Don't take ibuprofen or aspirin as these aren't recommended during pregnancy. If you need them, certain antibiotics are safe for pregnant women. Always read the patient information leaflet that comes with your medicine and if you have any questions, ask your pharmacist for advice.
Pregnancy hormones make your gums much more likely to bleed. It's important that you keep your teeth and gums healthy – make sure you clean your teeth twice a day and use dental floss and mouthwash if you need to. NHS dental care is free during pregnancy and for one year after, so you should make an appointment to see your dentist.
Further information
-
British Dental Health Foundation
0845 063 1188
www.dentalhealth.org.uk
Sources
- FAQ: Medical conditions and oral health. British Dental Health Foundation. www.dentalhealth.org.uk, accessed 22 June 2010
- Michalowicz BS, DiAngelis AJ, Novak MJ, et al. Examining the safety of dental treatment in pregnant women. J Am Dent Assoc 2008; 139(6):685–95. www.jada.ada.org
- X-rays: how safe are they? Health Protection Agency. www.hpa.org.uk, published May 2001
- The pregnancy book. Department of Health. www.dh.gov.uk, published October 2009
- Joint Formulary Committee, British National Formulary. 57th ed. London: British medial Association and Royal Pharmaceutical Society of Great Britain, 2009:818
Related topics
Local anaesthesia and sedation
General anaesthesia
Having a tooth removed
Further information
-
British Dental Health Foundation
0845 063 1188
www.dentalhealth.org -
British Association of Oral and Maxillofacial Surgeons
www.baoms.org.uk
Sources
- Removal of impacted wisdom teeth. British Association of Oral and Maxillofacial Surgeons. www.baoms.org.uk, published March 2007
- Management of unerupted and impacted third molar teeth. Section 4: Assessment and referral. Scottish Intercollegiate Guidelines Network (SIGN), 2000, SIGN Publication number 43. www.sign.ac.uk
- Is there any evidence that smoking impairs wound healing? Trip Answers. www.tripanswers.org, published February 2008
- Management of unerupted and impacted third molar teeth. Section 5: Clinical management. Scottish Intercollegiate Guidelines Network (SIGN), 2000, SIGN Publication number 43. www.sign.ac.uk
- What to do following an extraction. British Dental Health Foundation. www.dentalhealth.org.uk, accessed 22 June 2010
- Treatments: Tooth extraction. British Dental Association. www.bdasmile.org, accessed 22 June 2010
This information was published by Bupa's Health Information Team and is based on reputable sources of medical evidence. It has been peer reviewed by Bupa doctors. The content is intended for general information only and does not replace the need for personal advice from a qualified health professional.
Publication date: September 2010.