Type 2 diabetes
This factsheet is for people who have type 2 diabetes, or who would like information about it.
Type 2 diabetes is a lifelong condition in which the body can't control levels of glucose in the blood. It develops when the body can't make enough insulin or doesn't respond to it. Type 2 diabetes is sometimes called non-insulin dependent diabetes.
About type 2 diabetes
Symptoms of type 2 diabetes
Complications of type 2 diabetes
Causes of type 2 diabetes
Diagnosis of type 2 diabetes
Treatment of type 2 diabetes
About type 2 diabetes
Type 2 diabetes usually affects people over the age of 40, but can develop at any age. People of African-Caribbean or South Asian origin are more likely to develop type 2 diabetes and it usually affects them earlier in life, from about the age of 25. Type 2 diabetes is becoming more common, particularly in children.
Type 2 diabetes develops when your body can't produce enough insulin or if your body doesn't respond to insulin as it should. Insulin regulates the level of glucose in your blood. Glucose is a simple form of sugar found in foods and sugary drinks. It's absorbed by your body as a natural part of digestion and is carried around your body in your blood. When glucose reaches your body tissues, such as muscle cells, it's absorbed and converted into energy.
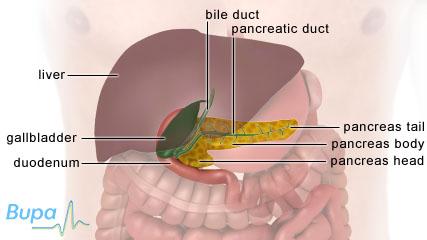
Insulin is secreted into your blood by your pancreas, which is a gland located behind your stomach. If your cells don't respond properly to insulin, it can cause glucose to build up in your blood. This is called insulin resistance. If this happens, your pancreas needs to produce more and more insulin to overcome the resistance and control your blood glucose levels.
Symptoms of type 2 diabetes
Many people with type 2 diabetes have no obvious symptoms.
If you do have symptoms of type 2 diabetes, you may:
- pass more urine than usual
- be constantly thirsty
- have unexplained weight loss
- be extremely tired
- have blurred vision
- have itchy skin around your genitals or get regular infections, such as thrush
- notice that wounds such as cuts heal slowly
If you have any of these symptoms, see a doctor.
Complications of type 2 diabetes
If type 2 diabetes isn't diagnosed or controlled properly, you can develop blood glucose levels that are either too high (hyperglycaemia) or too low (hypoglycaemia).
Hyperglycaemia
If type 2 diabetes is poorly controlled or if you get an infection, glucose can build up in your blood and rise to high levels. This can cause you to:
- be thirsty
- pass urine excessively
- have blurred vision
- feel tired
Very rarely, if you become dehydrated and your blood glucose rises to very high levels, you can develop a condition called hyperosmolar hyperglycaemic state. This can cause you to become drowsy and potentially unconscious. Hyperosmolar hyperglycaemic state is a medical emergency and needs to be treated in hospital.
In the long-term, uncontrolled high blood glucose levels can increase your risk of:
- kidney failure
- blindness
- nerve damage
- heart disease
- stroke
Hypoglycaemia
Sometimes, if your medication is too strong or you miss a meal, your blood glucose levels can become too low (hypoglycaemia). This only happens if you're taking certain medicines such as gliclazide (or others of the same type), repaglinide or insulin (of any type).
If your blood glucose is low, you may go pale, feel sweaty and become confused. If you develop hypoglycaemia, it's important to eat or drink something containing glucose, for example fruit juice or some sweets.
Causes of type 2 diabetes
There are several risk factors that make you more likely to develop type 2 diabetes, including if you:
- are overweight or obese – in particular, if you're an 'apple shape' with lots of fat around your abdomen (tummy)
- have a close family member with the condition
- are of African-Caribbean or of South-Asian origin
- are over 40 – your risk increases with age
- have high blood pressure or have had a heart attack or stroke
- don’t exercise regularly
- have severe mental health problems
- are a woman and have polycystic ovary syndrome and are overweight
- are a woman and have had diabetes that developed during pregnancy (gestational diabetes)
If you have a condition such as impaired glucose tolerance or impaired fasting glycaemia, these mean the level of glucose in your blood is naturally higher than normal and you're more likely to develop type 2 diabetes.
Diagnosis of type 2 diabetes
The doctor will ask about your symptoms and examine you. He or she may also ask about your medical history.
You may need to have some of the following tests.
- Urine test. You will need to give a sample to be tested for glucose.
- Fasting blood glucose test. You will have a sample of blood taken from your arm to test for glucose. You will need to fast overnight before having this test. You may have this with a glycosylated haemoglobin (HbA1C) test. HbA1C is a protein that is produced when you have high blood glucose levels over a long period of time.
- Glucose tolerance test. This may be needed if your fasting blood glucose test is borderline. It measures how your blood glucose level changes over time after you have a sugary drink. You will need to fast overnight before having this test.
Please note that availability and use of specific tests may vary from country to country.
Treatment of type 2 diabetes
There isn't a cure for type 2 diabetes but it can be controlled. Some people can control their condition with lifestyle changes alone. Others need to take medicines or use insulin injections.
Self-help
By making the following lifestyle changes, you can help control your blood glucose levels.
- Eat a healthy balanced diet with regular meals, three times a day. Include carbohydrates, such as pasta or potatoes in each meal.
- Try to do at least half an hour of moderate physical activity on at least three days a week. This will help you to stay a healthy weight and control your blood glucose levels.
- Only drink alcohol in moderation and stick within the recommended limits.
- If you smoke, give up. Smoking is unhealthy for everyone, but it's especially important to stop if you have diabetes because you already have an increased risk of developing circulatory problems and cardiovascular disease.
Oral medicines
If lifestyle changes alone don't keep your blood glucose levels under control, you may be prescribed medicines. Some examples are listed below.
- Metformin works by reducing the amount of glucose that gets released into your bloodstream from your liver. It also improves the way glucose is used by your muscles.
- Gliclazide, glipizide, glimepiride and tolbutamide help your pancreas to produce more insulin.
- Repaglinide and nateglinide also help your pancreas to produce more insulin, but work more quickly and last for a shorter time.
- Acarbose lowers your blood glucose by slowing down the rate at which some carbohydrates are absorbed by your body.
- Pioglitazone reduces your body's resistance to insulin.
- Sitagliptin, saxagliptin and vildagliptin help your body to produce more insulin at mealtimes.
These medicines are usually taken between one and three times a day.
Injections
You may be prescribed other medicines such as exenatide or liraglutide. These medicines are given by injection and work by helping your body to make more insulin when it's needed. They can also reduce your appetite and help you lose weight.
If lifestyle changes and medicines can't keep your blood glucose levels under control, you may need to have insulin injections as well as, or instead of, tablets.
You will usually inject yourself with insulin once or twice a day, using either a small needle or a pen-type syringe with replaceable cartridges. There are several different types of insulin that work at different rates and for different lengths of time. Ask your doctor for advice on which type is best for you.
If you have insulin injections, you will need to monitor your blood glucose levels with a home test kit. This involves taking a pinprick of blood from your finger and putting a drop on a testing strip. A meter will read the result automatically. Your doctor will show you how to monitor your blood glucose levels and tell you how often you need to check it.
Availability and use of different treatments may vary from country to country. Ask your doctor for advice on your treatment options.
Monitoring your blood glucose level
You may also need to have your levels of HbA1C tested at least twice a year. The test is done by taking blood from a vein in your arm or sometimes a drop of blood from a fingerprick. It's used to see how well you're controlling your blood sugar levels.
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email.
Will I be able to manage type 2 diabetes by myself?
Can I go on holiday if I have type 2 diabetes?
Are there any side-effects of using insulin for type 2 diabetes?
Will I be able to manage type 2 diabetes by myself?
Answer
Yes you can, and you will be encouraged to do so. Care for diabetes is planned around you and helping you to take control of your condition.
Explanation
You will be managing your diabetes as part of a team that includes your GP, practice nurse, and possibly a doctor or nurse who specialises in diabetes. You will usually have at least one full review of your condition every year. Outside of these visits to your doctor or nurse, you're likely to be looking after your condition yourself.
Your GP or nurse will discuss your treatment choices with you and help you to find the information and support you need to feel confident at home. If you’re having insulin injections, your GP or nurse may give you the option of monitoring your own blood glucose levels at home.
You might be invited to take part in a more structured diabetes education programme. There are lots of different courses available, depending on where you live. These courses are usually held in small groups. They aim to help you learn how to look after your condition and how to monitor it yourself.
One of these programmes is called DESMOND (Diabetes Education and Self Management for Ongoing and Newly Diagnosed). This is an educational programme specifically for people with type 2 diabetes. It's run for one full day or over two half days. It teaches you ways to manage your diabetes yourself and can help you to feel more in control of your condition.
Can I go on holiday if I have type 2 diabetes?
Answer
Yes, it's fine to go on holiday as long as you’re well prepared.
Explanation
People with diabetes travel all over the world and take the same kinds of holiday as people without diabetes. However, you must plan well before your trip and remember the following.
- Take extra supplies of your medication with you.
- If you're travelling across time zones, you may need to adjust your insulin schedule. Get advice from your doctor or nurse.
- If you become unwell when you're away, drink plenty of fluids and if you can't eat, make sure you have sugary drinks. If you can't eat or drink anything, go to hospital for treatment.
- Security regulations at airports may mean you have to make special arrangements to travel with insulin. Carry your diabetes identification and a letter from your doctor, and check with the airline you're flying with before you go.
- Declare your condition when you buy travel insurance and never travel without it.
If you have any questions or concerns about travelling, speak to your GP or diabetes specialist nurse.
Are there any side-effects of using insulin for type 2 diabetes?
Answer
Side-effects are the unwanted effects of a medicine. Insulin can have a number of different side-effects. It’s important to talk to your GP for advice.
Explanation
If you use insulin injections for diabetes, you may get swelling and bruising on and around the skin where you inject. You may also get a skin rash, but this is rare.
Insulin can cause fat to grow more quickly around the injection site, causing soft lumps to build up under your skin. It’s very important that you change injection sites regularly to prevent these lumps forming. Injection sites for insulin include your abdomen (tummy), thighs, bottom and sometimes your arms. You should also change the exact spot that you use within the injection site each time.
Hypoglycaemia (low blood glucose level) is a potential complication of insulin therapy. It can be caused if you take too much insulin. If you get hypoglycaemia, you may:
- feel shaky
- sweat
- be tired
- have blurred vision
- not be able to concentrate
- have headaches
- go pale
If this happens, you must eat or drink something sugary straightaway. Then eat something containing long-lasting carbohydrates such as a sandwich, some toast or a piece of fruit. Test your blood glucose level to see whether it's returning to normal. If it's not, call for emergency help immediately.
If you have any of these side-effects, it’s important to talk to your GP.
Further information
-
Diabetes UK
0845 120 2960
www.diabetes.org.uk
Sources
- Guide to diabetes. Diabetes UK. www.diabetes.org.uk, accessed 28 June 2011
- Type 2 diabetes: the management of type 2 diabetes. National Institute for Health and Clinical Excellence (NICE), 2008. www.nice.org.uk
- Diabetes mellitus. The Merck Manuals. www.merckmanuals.com, published June 2008
- DESMOND: Diabetes Education and Self management for Ongoing and Newly Diagnosed. Diabetes UK. www.diabetes.org.uk, published October 2005
- Diagnosis and management of type 1 diabetes in children, young people and adults. National Institute for Health and Clinical Excellence (NICE), 2004. www.nice.org.uk
- Joint Formulary Committee. British National Formulary. 61st ed. London: British Medical Association and Royal Pharmaceutical Society of Great Britain; 2011
- Simon C, Everitt H, van Dorp F. Oxford handbook of general practice. 3rd ed. Oxford: Oxford University Press, 2010: 352–53
- Personal communication, Dr Jonathan Katz, Consultant Endocrinologist, Barnet Hospital, 8 June 2011
- Kilpatrick ES, Winocour ES. ABCD position statement on haemoglobin A1C for the diagnosis of diabetes. Pract Diab Int 2010; 27(6):1–5.