Acne
This factsheet is for people who have acne, or who would like information about it.
Acne vulgaris, or acne, is a skin condition that causes spots. Acne can vary from mild to severe and usually affects the skin of the face, back and chest.
About acne
Symptoms of acne
Complications of acne
Causes of acne
Diagnosis
Treatment
About acne
More than four in five teenagers get some form of acne. It’s much less common in later life. However, about one in 20 women and one in 100 men aged 25 to 40 continue to be affected by acne, or develop it at this age (late-onset acne). Rarely, newborn babies can get acne in the first few weeks or months of life.
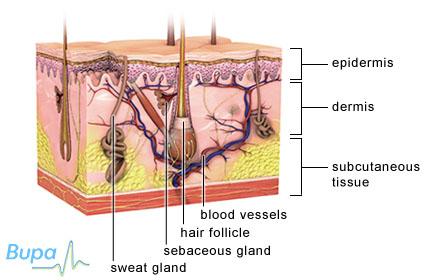
Acne starts to develop when hair follicles in your skin become blocked with the natural oil produced by your skin (known as sebum) and dead skin cells. Each follicle is connected to a sebaceous gland that lies just underneath the surface of your skin. The sebaceous glands produce sebum to keep your skin soft and supple. Normally, sebum travels up the follicle and out through small holes (pores) on the surface of your skin. However, if your body produces too much sebum, and dead skin cells get trapped in your pores, a ‘spot’ will form. This can either be a whitehead or a blackhead.
Sometimes the bacterium Propionibacterium acnes, which normally lives on the surface of your skin, causes inflammation (but not infection) in the hair follicles. If the inflammation develops near the surface of your skin, red or yellow spots (pustules) can form. Deeper inflamed lesions (nodules and cysts) can form if the infection is nearer the hair root. In very severe acne, cysts may join together to form even larger, deeper inflamed lesions (acne conglobata), but this is rare.
Acne isn't infectious, so you can't catch it or pass it on to other people.
Symptoms of acne
If you have mild or moderate acne, you may have greasy skin and spots (whiteheads or blackheads) on your face, back and chest. Most spots will not cause any other symptoms. Sometimes, spots that have become inflamed and infected (pustules, nodules and cysts) may be painful.
Acne can usually be treated with over-the-counter creams and lotions. However, if your acne doesn’t improve with self-help measures, or is affecting you emotionally, see your GP.
Complications of acne
Most people have a mild form of acne that usually clears up after their teenage years, but sometimes more severe complications may develop if you have moderate or severe acne.
- Scarring. Up to one in five people with acne have scarring that is socially noticeable. If you pick and squeeze your spots, you may get ‘ice pick’ scars. These are initially purple in colour before fading to a whitish colour. Rarely, ‘keloid’ (lumpy, painful and itchy) scars may develop on your chest and back.
- Hyperpigmentation (your skin becomes darker in the areas affected by acne). You’re more likely to have hyperpigmentation if you have a dark skin tone.
- Psychological problems. Acne may cause you to have low self-esteem or feel angry about the appearance of your skin, especially if you have scarring. Talk to your GP if your acne is making you feel particularly low.
Causes of acne
Contrary to popular belief, acne isn't caused by poor diet or bad hygiene.
During puberty, both men and women produce more of the male hormone testosterone. This increases the production of sebum in your skin, causing it to become greasy and encouraging spots to form. It’s thought that this is one of the main reasons most teenagers develop acne during puberty.
If you’re a woman, hormonal changes during your menstrual cycle and pregnancy may trigger acne.
Acne can be hereditary. For example, if both your parents had acne you have an increased chance of having it too.
Other rarer causes of acne may include:
- conditions such as polycystic ovary syndrome and Cushing’s syndrome
- some progesterone-based contraceptives
- cosmetic products, particularly some types of greasy moisturisers
- medicines such as steroid creams and ointments used for eczema, and some anti-epileptics
Diagnosis of acne
Your GP will examine your skin and may ask about your medical history.
Acne is easily recognisable by the distribution of spots on your body. Depending on how severe the acne is, your GP will recommend the most appropriate treatment.
Treatment of acne
Most treatments aim to control the symptoms of acne by:
- preventing new spots forming
- reducing inflammation in spots that are already present
- preventing scarring
Self-help
By keeping your skin clean you can help to prevent spots forming. Gently wash spot-prone areas with a mild soap or an unperfumed cleanser in lukewarm water about twice a day. Try not to wash the affected areas more than this, or scrub too hard, as your skin needs a certain amount of oil to maintain its natural condition. Acne isn’t an infection, so extra washing won’t help.
You may also be able to try an over-the-counter treatment that contains benzoyl peroxide (eg Oxy, Clearasil) – this has an antibacterial action and encourages your skin to shed its surface layer of dead cells. Together, these effects reduce the inflammation in existing spots and prevent new ones forming. These treatments are available from pharmacies and larger supermarkets.
Treatments containing benzoyl peroxide may cause your skin to become irritated (slightly reddened), especially to start with. This tends to settle down if you reduce the number of times you use it. You can then build up your use gradually.
Self-help treatments for acne take time to improve your skin noticeably, so it’s important not to expect a big difference overnight. Your acne may only get better several months after you have been using the treatment regularly.
Creams and lotions
If your acne hasn’t improved with self-help measures after about two months, see your GP. He or she may prescribe one of the following treatments.
- Azelaic acid – this is an antibacterial medicine usually used as an alternative to benzoyl peroxide, as it’s less likely to make your skin as red, or peel as much.
- Retinoids such as tretinoin and isotretinoin – these are medicines based on vitamin A that work by unblocking your pores. You should avoid the sun if you’re using retinoids as they can make your skin more prone to redness, stinging and dryness. You shouldn’t use retinoids if you’re pregnant or breastfeeding as they can cause harm to your baby (teratogenic).
- Antibiotic lotions, such as erythromycin or clindamycin – these can help control the P. acnes bacteria on your skin.
You will usually be advised to continue with your treatment for two months. If your acne has not improved after this time, your doctor may advise trying an oral treatment (a medicine you take by mouth).
Oral antibiotics
If you have moderate acne, your doctor may prescribe an antibiotic such as tetracycline or doxycycline. Your GP will advise you how many times a day you need to take your medicine, but you will need to stay on the course for a minimum of eight weeks. You may find it takes up to six months for your skin to improve and if your acne is severe, you may need to continue treatment for two years or longer. You may also need to apply a cream or lotion containing benzoyl peroxide to increase the effectiveness of your antibiotic treatment.
Oral contraceptives
If you’re a woman and treatments with oral antibiotics haven’t worked, your GP may advise taking an oral contraceptive pill, which combines a hormone called ethinyloestradiol with cyproterone acetate (eg Dianette). These medicines suppress the male hormones which are responsible for increasing sebum production.
Oral retinoids
If you have severe acne, or acne that has proven resistant to other treatments, your GP may refer you to a dermatologist (a doctor specialising in skin conditions) for treatment with an oral retinoid (eg isotretinoin). These medicines are very effective at reducing the amount of sebum your skin produces.
You will probably be asked to have a fasting blood test, which means you shouldn’t eat anything for up to 12 hours beforehand. You shouldn’t have any other fluids except water to drink. This test is used to measure your blood lipid levels (cholesterol) and liver function before you start treatment. Depending on the opinion of your dermatologist, you may need to have further fasting blood tests during treatment.
If you’re a woman, you should try to use two effective forms of contraception for at least one month before treatment, as well as during treatment, and for at least one month after stopping. This is because oral retinoids are teratogenic. So for safety reasons, you will be asked to take regular pregnancy tests and will be limited to one month’s supply of the medicine.
Oral retinoids have a number of unpleasant side-effects, including skin dryness, nose bleeds and joint pains. They can also occasionally make people feel down or depressed. If you ever had these symptoms in the past, you must let your dermatologist know before you start treatment. It’s also recommended that you keep your alcohol intake to a minimum when you’re being treated with isotretinoin.
You will have the opportunity to fully discuss all of these issues and ask any questions you may have with your dermatologist before you start treatment.
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email.
What's the best way to apply benzoyl peroxide?
I’ve heard oral retinoids are very effective at treating acne. Can I be prescribed them?
Does sunlight help acne?
What's the best way to apply benzoyl peroxide?
You should apply products that contain benzoyl peroxide once or, if necessary, twice a day. Benzoyl peroxide is available in several different formulations. You may find some suit you better than others.
Explanation
Benzoyl peroxide is available to buy over-the-counter on its own as a cream, a gel or a wash. It's worth trying different types and seeing which works best for you. For example, you may find some formulations, such as the wash, are better suited to treating the spots on your chest or back. Others (eg creams or gels), may be easier to apply on your face.
Before you apply the benzoyl peroxide treatment, you should wash your face with a mild soap and lukewarm water and leave it to dry for 20 minutes. It’s important to dry your skin properly before applying the treatment as otherwise these products can cause a surface layer to form on your skin, which later peels. You should then put the treatment on all areas affected by acne, not just on the places where you have spots. Don’t use too much – for example, a pea-sized amount of cream should be enough to cover your face. Areas that have cleared of acne should also be treated until the whole area has settled down. You may need to repeat this once or twice a day.
Benzoyl peroxide may cause your skin to become irritated (slightly red, itchy and scaly) when you first use it. However, if you reduce the number of times you use it, but apply regularly, the irritation should improve. Alternatively, you may need to use a lower strength treatment.
Always read the patient information leaflet that comes with your medicine and if you have any questions, ask your pharmacist for advice.
Further information
-
British Association of Dermatologists
020 7383 0266
www.bad.org.uk
Sources
- Acne vulgaris. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 22 July 2010
- Personal communication, Dr Mike Ardern-Jones, Consultant Dermatologist, Spire Southampton Hospital, 16 August 2010
- Joint Formulary Committee, British National Formulary. Acne. 59th ed. London: British Medical Association and Royal Pharmaceutical Society of Great Britain, 2010:13.6.1
I’ve heard oral retinoids are very effective at treating acne. Can I be prescribed them?
Acne can usually be controlled with creams, lotions and antibiotics. However, severe acne, and acne that has not responded to other treatments, may sometimes be treated with retinoid tablets.
Oral retinoids can only be prescribed by a dermatologist (a doctor who specialises in skin conditions).
Explanation
Oral retinoids can be very effective at treating acne. They work by reducing the amount of oil that sebaceous glands produce, as well as acting as an anti-inflammatory and reducing the presence of the P. acnes bacteria on your skin.
Oral retinoids are only prescribed if:
- you have severe acne, especially if it's causing nodules or cysts
- the acne cysts have started to join together beneath your skin,
- your skin is scarring,
- your acne hasn't responded to previous courses of oral and topical antibiotics,
- your acne is causing you psychological problems,
However, oral retinoids have many unpleasant and potentially serious side-effects. The most common side-effects are dry skin, nosebleeds, headaches and muscle aches. Some people taking oral retinoids have reported mood changes such as depression, anxiety, aggressive behaviour or suicidal thoughts, but these are rare. For this reason, an oral retinoid is only used as a last resort and your dermatologist may not prescribe it if you have a history of mental illness.
Further information
-
British Association of Dermatologists
020 7383 0266
www.bad.org.uk
Sources
- Acne vulgaris. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 22 July 2010
- Acne vulgaris. emedicine. www.emedicine.medscape.com, published 21 June 2010
- Joint Formulary Committee, British National Formulary. Acne. 59th ed. London: British Medical Association and Royal Pharmaceutical Society of Great Britain, 2010:13.6.1
Does sunlight help acne?
Sunlight may help some people with acne, but this isn’t predictable and won’t improve all cases of acne. The risk of getting skin cancer as a result of damage from the sun’s rays far outweighs any improvements to acne.
Explanation
Some people find that sunlight improves their acne in the short term, but there aren’t thought to be any long-lasting benefits.
Although some studies have suggested artificial ultraviolet (UV) light therapy can slightly improve acne, these haven’t been conclusive and are being investigated further. However, as there is strong and clear evidence that repeated sunbed use and excessive exposure to sunlight increase your risk of getting skin cancer, UV-based therapies aren’t recommended as a treatment for acne.
Talk to your GP for more advice. You should never allow yourself to burn if you’re in the sun and should always use sunscreen. If you're using sunscreen on sites prone to acne, it's important to use non-comedogenic (or acne friendly) preparations.
Further information
-
British Association of Dermatologists
020 7383 0266
www.bad.org.uk
Sources
- Acne vulgaris. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 22 July 2010
- Personal communication, Dr Mike Ardern-Jones, Consultant Dermatologist, Spire Southampton Hospital, 16 August 2010
Related topics
Depression
Eczema
Impetigo
This information was published by Bupa’s Health Information Team and is based on reputable sources of medical evidence. It has been peer reviewed by Bupa doctors. The content is intended for general information only and does not replace the need for personal advice from a qualified health professional.
Publication date: September 2010
Acne factsheet
Visit the acne health factsheet for more information.
Related topics
Depression
Eczema
Impetigo
Further information
British Association of Dermatologists
020 7383 0266
www.bad.org.uk
Sources
- Acne vulgaris. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 22 July 2010
- Simon C, Everitt H, van Dorp F. Oxford handbook of general practice. 3rd ed. Oxford: Oxford University Press, 2010:620–21
- Acne vulgaris. emedicine. www.emedicine.medscape.com, published 21 June 2010
- Acne vulgaris. Merck Online Medical Library. www.merck.com/mmpe, published August 2008
- Personal communication, Dr Mike Ardern-Jones, Consultant Dermatologist, Spire Southampton Hospital, 16 August 2010
- Joint Formulary Committee, British National Formulary. Acne. 59th ed. London: British Medical Association and Royal Pharmaceutical Society of Great Britain, 2010:13.6.1
- Cholesterol. Lab Tests Online. www.labtestsonline.org, published 18 June 2010
This information was published by Bupa’s Health Information Team and is based on reputable sources of medical evidence. It has been peer reviewed by Bupa doctors. The content is intended for general information only and does not replace the need for personal advice from a qualified health professional.
Publication date: September 2010.














