Cardioversion
[Published by Bupa’s health information team, June 2010.]
This factsheet is for people who are planning to have cardioversion, or who would like information about it.
Cardioversion uses medicine and/or an electric shock to help the heart return to its normal rhythm. This factsheet focuses on DC cardioversion.
You will meet the doctor carrying out your procedure to discuss your care. It may differ from what is described here as it will be designed to meet your individual needs.
About cardioversion
Diagnosis of heart conditions
What are the alternatives to cardioversion?
Preparing for cardioversion
About the procedure
What to expect afterwards
Recovering from cardioversion
What are the risks?
About cardioversion
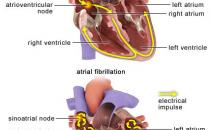
Arrhythmia (irregular heartbeat) is caused by faulty electrical signals in your heart. Your doctor may recommend cardioversion as a treatment for some types of arrhythmia, such as:
• atrial fibrillation – when the heart beats too fast or irregularly
• atrial flutter – when the heart may not always beat irregularly but beats too fast
• ventricular tachycardia – when the heart beats too fast
There are two types of cardioversion – medical and electrical.
• Medical cardioversion – anti-arrhythmic medicines are used to control your heart rate and rhythm. Medicines are usually given by injection within 48 hours of having symptoms. These can include medicines, such as amiodarone, flecainide and sotalol.
• Electrical (DC) cardioversion – an electric shock is used to help your heart beat at normal rhythm. It’s usually given if your arrhythmia has lasted longer than 48 hours. DC cardioversion is less likely to work if the arrhythmia has been present for over a year. It’s also not suitable if the irregular rhythm is coming and going, since it’s most likely that the arrhythmia will return after DC cardioversion.
Your doctor will decide if DC cardioversion is suitable, depending on how long your heart has been beating irregularly, your general symptoms and your medical history.
Sometimes an anti-arrhythmic medicine is used with DC cardioversion to help maintain a regular heartbeat. This may be needed if DC cardioversion hasn’t worked or the rhythm problem returns after treatment. If this happens, you will usually have to take anti-arrhythmic medicines for four weeks before and after having a repeat DC cardioversion.
With ventricular tachycardia you can be very unwell, so DC cardioversion is often done urgently to correct the heart rhythm.
What are the alternatives to cardioversion?
There are many treatments other than DC cardioversion available to help regulate the heart’s rhythm. Some are listed below.
• Anti-arrhythmic medicines – usually given as tablets – can help control your heart rate and rhythm, but this may take several days or weeks to take effect.
• Surgery (ablation) – a special sensor is passed from the vein in the groin up to the heart. Unusual tissue which may be disrupting the electrical signals in your heart is then frozen or burnt.
• Pacemaker – this helps regulate the heartbeat. It’s usually only used after the AV node (where the heart’s electrical signals pass through) has been destroyed on purpose using ablation.
Your doctor will advise which treatment is most suitable for you.
Preparing for cardioversion
Your doctor will explain how to prepare for your DC cardioversion. You will have blood tests to check your blood count, kidney function and how your blood clots.
Your doctor may prescribe:
• anticoagulant medicines – these help to stop blood clotting (usually warfarin is used)
• anti-arrhythmic medicines – to help regulate your heart’s rhythm
DC Cardioversion is routinely done as an out-patient or day case, under sedation or light general anaesthesia. Sedatives help you feel relaxed and drowsy whereas general anaesthesia puts you to sleep during the procedure.
If you’re having a general anaesthetic, you will be asked to follow fasting instructions. Typically you must not eat or drink for about six hours before a general anaesthetic. However, some anaesthetists allow occasional sips of water until two hours beforehand.
You’re likely to have the following hospital tests before DC cardioversion.
• Electrocardiogram (ECG) – measures the electrical activity in your heart to see what the heart rhythm is.
• Echocardiogram – an ultrasound scan of your heart provides a clear image of your heart muscles and valves that shows how well the heart is working.
• Transoesophageal echocardiogram (TOE) – this is done if you’re unable to take anticoagulant medicines or if you have only developed the irregular heartbeat within the last 48 hours. A small sensor is put into your oesophagus (gullet) to scan for blood clots in the heart.
Your doctor will discuss with you what will happen before, during and after your procedure, and any pain you might have. This is your opportunity to understand what will happen, and you can help yourself by preparing questions to ask about the risks, benefits and any alternatives to the procedure. This will help you to be informed, so you can give your consent for the procedure to go ahead, and you may be asked to sign a consent form.
About the procedure
DC cardioversion usually takes five to 10 minutes. Following sedation or general anaesthesia your doctor will give a brief, controlled electric shock to your heart usually through two pads placed on your chest.
Your heart rate and rhythm is monitored throughout the procedure, and your doctor can see immediately if the procedure has reset your heart to its normal rhythm.
Your doctor may give you up to two more electric shocks to reset the heart if the first attempt is unsuccessful.
What to expect afterwards
If you have general anaesthesia, you will need to rest until the effects of the anaesthetic have passed.
Your nurse will regularly check your heart rate and blood pressure. You will be able to go home once your heart rhythm is stable and you have fully recovered.
Your doctor may prescribe anticoagulant and anti-arrhythmic medicines for you to take at home.
You will need to arrange for someone to drive you home. After general anaesthesia, you should try to have a friend or relative stay with you for the first 24 hours.
If the cardioversion hasn’t worked, then your doctor may discuss other treatment options with you. Your doctor may arrange for you to come back at a later date for further treatment.
You will usually be given a date for a follow-up appointment before you go home.
Recovering from cardioversion
General anaesthesia (and sedation) temporarily affect your coordination and reasoning skills, so you must not drive, drink alcohol, operate machinery or sign legal documents for 48 hours afterwards (24 hours after sedation). If you’re in any doubt about driving, contact your motor insurer so that you’re aware of their recommendations, and always follow your doctor’s advice.
You should limit your alcohol, tobacco and caffeine intake, especially after having cardioversion treatment, as these are stimulants and can speed up your heart rate.
Contact your GP if you feel any changes in your heartbeat.
What are the risks?
Cardioversion is commonly performed and generally safe. However, in order to make an informed decision and give your consent, you need to be aware of the possible side-effects and the risk of complications.
Side-effects
Side-effects are the unwanted but mostly temporary effects you may get after having the procedure, for example feeling sick as a result of the general anaesthetic.
The skin on your chest may feel a little sore where the shock was administered after having DC cardioversion.
Cardioversion can cause a temporary drop in blood pressure, so you may have:
• headache
• dizziness
• flushing
The anti-arrhythmic medicine amiodarone can cause problems with your thyroid gland, lungs and liver; and make your skin very sensitive to sunlight. If you’re prescribed amiodarone, you will have regular check-ups and will need to wear sunscreen and cover-up in the sun more than usual.
Complications
Complications are when problems occur during or after the procedure.
The most common complication of DC cardioversion is failure to restore normal rhythm. The success of cardioversion depends on your medical condition. Research shows cardioversion immediately restores the heart’s normal rhythm in nine in 10 people with arrhythmia. However, up to two in 10 people find that their heart’s rhythm becomes irregular again within a few days, and up to seven in 10 within the first year.
Your doctor will usually prescribe medicines to help maintain a regular heartbeat. Your doctor may arrange for you to come back at a later date for further treatment if the procedure isn’t successful.
Other possible complications of DC cardioversion include:
• an unexpected reaction to the anaesthetic – medicines are available to help if this happens
• heart rhythm problems – sometimes unusual slow or fast heart beats can occur during cardioversion and medicines are available to help if this happens
• heart attack or stroke – this is very unusual, anticoagulant medicines are used to reduce the risk of blood clots forming
The exact risks are specific to you and differ for every person so we have not included many statistics. Ask your doctor to explain how these risks apply to you.
Why do I need anticoagulant medicines before having a cardioversion?
Why do I need medicines to help regulate my heart rhythm after cardioversion?
Is there a limit to how many times you can have cardioversion for arrhythmia?
Why do I need anticoagulant medicines before having a cardioversion?
Anticoagulant medicines are prescribed to help reduce your risk of developing a blood clot.
Explanation
If you have arrhythmia, it means you have an irregular heart beat. Because of this blood may start to pool in the chambers of your heart and form a clot. The blood clot can block circulation in your heart and cause a heart attack. If it moves through the bloodstream to the brain, it could cause a stroke.
Your doctor will usually prescribe anticoagulant medicine (usually warfarin) to help reduce your risk of developing a blood clot. You will usually be asked to take this for at least three weeks before, during and for four weeks after having cardioversion.
Further information
The British Heart Foundation
0300 330 3311
www.bhf.org.uk
Source
• Atrial fibrillation. National Institute for Health and Clinical Excellence (NICE), June 2006. www.nice.org.uk
Why do I need medicines to help regulate my heart rhythm after cardioversion?
Medicines to help regulate heart rate and rhythm are usually prescribed if DC cardioversion doesn’t work or the arrhythmia comes back after a previous treatment.
Explanation
Arrhythmia can return at any time after a successful cardioversion. Re-occurrence is most common in the first two weeks after having cardioversion.
Studies suggest DC cardioversion is more likely to succeed and arrhythmia is less likely to re-occur if anti-arrhythmic medicines such as amiodarone and sotalol are used. Anti-arrhythmic medicines help control the heart rate and rhythm.
You’re more likely to have anti-arrhythmic medicines if cardioversion hasn’t worked or if your arrhythmia returns after a previous attempt.
These medicines are not used routinely with a first DC cardioversion attempt because of their side-effects. However, your doctor may recommend using them if he or she thinks the DC cardioversion is less likely to work. For example, electrical cardioversion is less likely to succeed if you have had arrhythmia for a long time.
Further information
The British Heart Foundation
0300 330 3311
www.bhf.org.uk
Sources
• Atrial fibrillation. National Institute for Health and Clinical Excellence (NICE), June 2006. www.nice.org.uk
• Atrial fibrillation. British Heart Foundation. www.bhf.org.uk. published June 2009
• Sulke N, Sayers F, Lip GYH. Rhythm control and cardioversion. Heart 2007; 93:29–34, doi:10.1136/hrt.2006.099879, accessed 18 March 2010
• Adgey AAJ, Walsh SJ. Theory and practice of defibrillation: (1) Atrial fibrillation and DC conversion. Heart 2004; 90:1493–98, doi:10.1136/hrt.2003, accessed 18 March 2010
• Atrial fibrillation. Arrhythmia Alliance. www.heartrhythmcharity.org.uk, accessed 30 March 2010
• Medicines for the Heart. British Heart Foundation. www.bhf.org.uk, published June 2009
Is there a limit to how many times you can have electrical cardioversion for arrhythmia?
You’re likely to be offered a second cardioversion treatment if your arrhythmia returns after a previous successful procedure. If your arrhythmia returns again, your doctor is likely to suggest alternative treatments to correct your arrhythmia.
Explanation
It’s possible that the DC cardioversion may fail to correct your heart rhythm. It's also possible that the arrhythmia may return at any time after a successful cardioversion. Re-occurrence is most common in the first two weeks after having cardioversion.
Research suggests DC cardioversion may be attempted again if a previous attempt has not worked or if arrhythmia returns after a successful procedure.
You’re likely to be offered a second DC cardioversion if your arrhythmia returns after a previous successful procedure. With your second treatment, your doctor will most likely prescribe medicines to help control your heart rhythm to avoid a further relapse.
If your arrhythmia returns again, your doctor is likely to suggest alternative treatments to correct your arrhythmia.
Further information
The British Heart Foundation
0300 330 3311
www.bhf.org.uk
Sources
• Atrial fibrillation. National Institute for Health and Clinical Excellence (NICE), June 2006. www.nice.org.uk
• Atrial fibrillation. British Heart Foundation. www.bhf.org.uk. published June 2009
• Sulke N, Sayers F, Lip GYH. Rhythm control and cardioversion. Heart 2007; 93:29–34, doi:10.1136/hrt.2006.099879, accessed 18 March 2010
• Adgey AAJ, Walsh SJ. Theory and practice of defibrillation: (1) Atrial fibrillation and DC conversion. Heart 2004; 90:1493–98, doi:10.1136/hrt.2003, accessed 18 March 2010
• Atrial fibrillation. Arrhythmia Alliance. www.heartrhythmcharity.org.uk, accessed 30 March 2010
• Medicines for the heart. British Heart Foundation. www.bhf.org.uk, published June 2009
Related topics
• Arrhythmia (palpitations)
• Beta-blockers
• Echocardiogram
• Electrocardiogram
[standard disclaimer and publication date]
Cardioversion factsheet
Visit the cardioversion health factsheet for more information.
Related topics
• Arrhythmia (palpitations)
• Beta-blockers
• Echocardiogram
• Electrocardiogram
• General anaesthesia
Further information
The British Heart Foundation
0300 330 3311
www.bhf.org.uk
Sources
• Atrial fibrillation. National Institute for Health and Clinical Excellence (NICE), June 2006. www.nice.org.uk
• What is an arrhythmia? National Heart Lung and Blood Institute.
www.nhlbi.nih.gov, accessed 18 March 2010
• Atrial fibrillation. British Heart Foundation. www.bhf.org.uk. published June 2009
• Sulke N, Sayers F, Lip GYH. Rhythm control and cardioversion. Heart 2007; 93:29–34, doi:10.1136/hrt.2006.099879, accessed 18 March 2010
• Adgey AAJ, Walsh SJ. Theory and practice of defibrillation: (1) Atrial fibrillation and DC conversion. Heart 2004; 90:1493–98, doi:10.1136/hrt.2003, accessed 18 March 2010
• Atrial fibrillation. Arrhythmia Alliance. www.heartrhythmcharity.org.uk, accessed 30 March 2010
• Medicines for the Heart. British Heart Foundation. www.bhf.org.uk, published June 2009
• Amiodarone. British National Formulary 59. http://bnf.org, accessed 18 March 2010
• Cardioversion of atrial fibrillation. Atrial Fibrillation Association. www.atrialfibrillation.org.uk, published 2008
• Personal communication. Dr Timothy Cripps DM, FRCP. Consultant Cardiologist, University Hospitals Bristol Foundation Trust, Bristol, UK. April 2010.