Ectopic pregnancy
Published by Bupa's Health Information Team, March 2010.
This factsheet is for women who may have an ectopic pregnancy or people who would like information about it.
An ectopic pregnancy is when a fertilised egg implants outside the womb, most often in one of the fallopian tubes. It's not possible for pregnancy to survive outside the womb and immediate treatment may be needed.
About ectopic pregnancy
Symptoms of ectopic pregnancy
Causes of ectopic pregnancy
Diagnosis of ectopic pregnancy
Treatment of ectopic pregnancy
Prevention of ectopic pregnancy
About ectopic pregnancy
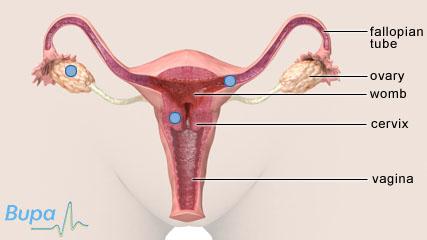
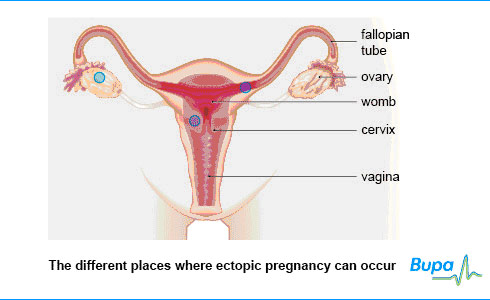
In a normal pregnancy, an egg released by your ovary is fertilised in one of your fallopian tubes and travels to your womb where it implants in the womb lining. If you have an ectopic pregnancy, it means the fertilised egg has implanted somewhere other than in your womb. It is most likely to happen in one of your fallopian tubes (called a tubal pregnancy). However, the fertilised egg can also implant:
- at the point where your fallopian tube meets your womb
- on one of your ovaries
- at the neck of your womb (cervix)
- in your abdomen
Ectopic pregnancy occurs in about one in every 100 pregnancies.
Symptoms of ectopic pregnancy
The symptoms of ectopic pregnancy are different in all women. However, the most common symptoms include the following.
- Pain in your abdomen, usually on one side. This can be mild to extremely severe. It may come on over a few days or suddenly without any warning.
- Unusual bleeding from your vagina. This may be heavier or lighter than your usual monthly period, and it may be a different colour.
- Missing your monthly period. However, you may not have noticed this if the pregnancy takes place very early on in the menstrual cycle, or if you have had any other bleeding that you may have mistaken for your period.
- Pain in the tip of your shoulder. If your fallopian tube tears (ruptures), it can cause bleeding into your abdomen, which can irritate the diaphragm (the sheet of muscle that lies between your abdomen and your chest). Your diaphragm shares nerves with those running to your shoulder, so you may feel pain from your diaphragm in your shoulder.
- Feeling faint. If your fallopian tube ruptures, you may have a serious internal bleed causing you to suddenly collapse, feel dizzy or faint.
- Pain on having a bowel movement or passing urine.
If you have missed a period or could be pregnant and have any of the symptoms above, see a doctor straight away.
Causes of ectopic pregnancy
Ectopic pregnancy usually develops because your fallopian tubes have become damaged. This could have happened during an earlier operation on your abdomen or if you have had pelvic inflammatory disease, which is usually caused by a sexually transmitted infection, such as chlamydia or gonorrhoea. If your fallopian tubes have been damaged, they may become inflamed, narrowed or scarred, which makes it harder for the fertilised egg to pass down to your womb.
Other things that make an ectopic pregnancy more likely include:
- smoking
- being treated for infertility
- a previous ectopic pregnancy
However, for many ectopic pregnancies, the cause is unknown.
Diagnosis of ectopic pregnancy
Your doctor will ask about your symptoms and examine you. He or she may also ask you about your medical history.
Your doctor will usually ask you to do a pregnancy test. The pregnancy test involves testing a sample of your urine for a hormone called human chorionic gonadotrophin (hCG). This hormone is made by the cells that form the placenta.
If the test is positive, you may have a blood test for hCG and an ultrasound scan. Ultrasound uses sound waves to produce an image of the inside of part of your body. If the scan shows that your womb is empty but your blood test shows high levels of hCG, it’s very likely that you have an ectopic pregnancy.
If your doctor is still unsure, you may need to have a procedure called a laparoscopy. Your doctor will use a narrow, tube-like telescopic camera (called a laparoscope) to look inside your fallopian tubes. The laparoscope is inserted into your abdomen through a small cut. You will usually have a general anaesthetic. This means that you will be asleep during the procedure and feel no pain.
Treatment of ectopic pregnancy
The treatment for ectopic pregnancy depends on how severe your symptoms are, how advanced your pregnancy is and whether or not your fallopian tube has ruptured.
Watchful waiting
Some ectopic pregnancies don’t need to be treated because the pregnancy ends by itself. If you don’t have any symptoms, or your symptoms are only mild, you may be given the option of not having any treatment. Instead, your doctor will want to monitor you closely using blood tests and further ultrasound scans.
Medicines
If it’s confirmed that the ectopic pregnancy is in one of your fallopian tubes and it’s still early on in the pregnancy, your doctor may recommend that you have an injection of a medicine called methotrexate. This disrupts the pregnancy and causes it to end. You may need to have more than one dose. However, the medicine isn’t always effective at preventing your fallopian tube from rupturing. If it does, you will need to have surgery.
Surgery
You may need surgery to remove your ectopic pregnancy if:
- medical treatment hasn’t worked
- your pregnancy is quite advanced or located outside your fallopian tubes
- your fallopian tube has ruptured and you have a severe internal bleed
You may have keyhole surgery (laparoscopy) or open surgery (laparotomy) for ectopic pregnancy. However, open surgery is more likely if your fallopian tube has ruptured. Depending on where your pregnancy is and how advanced it is, your surgeon may remove the pregnancy by using a device to suck (aspirate) it out of the fallopian tube, or by removing part or all of the fallopian tube.
You may need a blood transfusion if you have a severe internal bleed or open surgery.
Prevention of ectopic pregnancy
It isn’t possible to prevent an ectopic pregnancy as it can affect any woman. However, you can reduce your risk of having an ectopic pregnancy if you take measures to protect yourself against sexually transmitted infections, which can damage your fallopian tubes, and quit smoking.
It is normal to experience emotional reactions, including feelings of sadness and a sense of loss after having an ectopic pregnancy and it’s important that you try to talk to someone close about these feelings.
Will I be able to get pregnant again after an ectopic pregnancy?
If it’s left to develop, could an ectopic pregnancy turn into a successful one?
Is it true that using the coil for contraception increases your risk of ectopic pregnancy?
Will I be able to get pregnant again after an ectopic pregnancy?
Yes, but it may be more difficult.
Explanation
If you have had an ectopic pregnancy, it’s possible that you will have more trouble getting pregnant again than a woman who hasn’t had one. You’re also more likely to have another ectopic pregnancy. Around two-thirds of women who have had an ectopic pregnancy will become pregnant again. Of these, about one in 10 will have another ectopic pregnancy.
These problems are caused because one of your fallopian tubes is likely to have been damaged or even removed. However, as surgical methods have advanced and treatment with methotrexate is becoming more common, fewer women are having problems with subsequent pregnancies.
Further information
The Ectopic Pregnancy Trust
020 7733 2653
www.ectopic.org.uk
Source
- A detailed account of ectopic pregnancies. The Ectopic Pregnancy Trust. www.ectopic.org.uk, accessed 24 November 2009
If it’s left to develop, could an ectopic pregnancy turn into a successful one?
No, ectopic pregnancies are not able to develop properly, so it would never be possible for an ectopic pregnancy to survive.
Explanation
It isn’t possible for a pregnancy to survive if it implants outside the womb. Only the womb provides the right environment for the baby to grow and receive all the nutrition it needs before it’s born.
If the pregnancy implants in your fallopian tube, there is a risk that it will cause it to tear (rupture). This can cause severe bleeding and if left untreated, can be life-threatening.
Because an ectopic pregnancy can’t survive, the most important thing to consider when deciding on treatment is your health.
Further information
The Ectopic Pregnancy Trust
020 7733 2653
www.ectopic.org.uk
Sources
- Ectopic and Molar Pregnancy. March of Dimes. www.marchofdimes.com, accessed 24 November 2009
Is it true that using the coil for contraception increases your risk of ectopic pregnancy?
No, but if you do become pregnant even though you have had the coil fitted, you are at a slightly increased risk of ectopic pregnancy.
Explanation
The risk of having an ectopic pregnancy when you have had an intra-uterine contraceptive device (coil) fitted is lower than if you don’t use any contraception. However, even though it’s very unlikely, if you have had a coil fitted, you may still become pregnant. If this happens, you are slightly more at risk of ectopic pregnancy – about one in 20 women who become pregnant with a coil in place have an ectopic pregnancy. This is because the coil is good at stopping pregnancies from implanting in the womb but it isn’t as good at preventing conception in the fallopian tubes.
Further information
The Ectopic Pregnancy Trust
020 7733 2653
www.ectopic.org.uk
Sources
- Ectopic and Molar Pregnancy. March of Dimes. www.marchofdimes.com, accessed 24 November 2009
- A detailed account of ectopic pregnancies. The Ectopic Pregnancy Trust. www.ectopic.org.uk, accessed 24 November 2009
- The management of tubal pregnancy. Royal College of Obstetricians and Gynaecologists, 2004, Guideline 21. www.rcog.org.uk, accessed 25 November 2009
- Tay JI, Moore J, Walker JJ. Ectopic pregnancy. BMJ 2000; 320:916-19. www.bmj.com
- Arulkumaran S, Symonds IM, Fowlie A. Oxford Handbook Obstetrics and Gynaecology. Oxford University Press 2004:513-17
- IUD use and the risk of ectopic pregnancy: a meta-analysis of case-control studies. Database of abstracts of reviews of effects. May 1998. www.crd.york.ac.uk, accessed 24 November 2009
- Tay JI, Moore J, Walker JJ. Ectopic pregnancy. West J Med 2000; 173(2):131–34.
Visit the ectopic pregnancy health factsheet for more information
Related topics
Contraception – non-hormonal
















