Food allergy

Published by Bupa's Health Information Team, August 2010.
This factsheet is for people who have a food allergy, or who would like information about them.
A food allergy is when the body's immune system mistakes particular foods, for example eggs or nuts, as harmful. Most food allergy reactions are mild, but sometimes they can be very serious and even fatal.
About food allergies
Symptoms of food allergy
Complications of food allergy
Causes of food allergy
Diagnosis of food allergy
Treatment of food allergy
About food allergies
In the UK, food allergies affect about one to two people in every 100. Food allergy is sometimes confused with food intolerance or food poisoning. These can make you feel ill but they aren't usually harmful in the same way that a true food allergy might be.
Foods that cause allergies include peanuts, tree nuts (Brazils, almonds, cashews, hazelnuts, walnuts and pecans), fish and shellfish, cows' milk, eggs, soya and wheat.
Food allergies in young children are more common than in adults, but many children outgrow them by school-age. It's possible to develop a food allergy as an adult, even if you never had allergies as a child.
If you have one food allergy, you may also react to other foods. For instance, if you're allergic to prawns, other shellfish may also affect you. People with hay fever or an allergy to latex may also find their allergic reaction crosses over and happens with certain foods. This is called cross-reactivity.
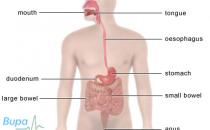
Food and the immune system
If you have an allergy, it means that your body's immune system reacts to an allergen – a substance that causes an allergic reaction. An allergic reaction happens when your body's immune system mistakes the allergen, for example nuts, for a harmful invader and produces antibodies. This is known as sensitisation and may not cause symptoms. However, the next time you eat the food, the antibodies are ready to react with it. This causes your body to release chemicals, which leads to a range of physical symptoms known as an allergic reaction. Allergens aren't usually harmful and most people aren't sensitive to them.
Symptoms of food allergy
Some food allergies result in immediate, severe and even life-threatening symptoms (such as severe peanut allergy), whereas others cause symptoms that may take longer to develop (for example, gluten allergy, also known as coeliac disease).
If you have a food allergy, you may have symptoms that include:
• itchy or swollen lips, mouth, tongue and throat
• skin reactions (eg swelling and itching, a rash around your mouth, eczema and flushing)
• wheezing or shortness of breath
• diarrhoea, feeling sick, vomiting and bloating
• coughing
• a runny nose
• sore, red and itchy eyes
These symptoms may be caused by problems other than a food allergy. If you have any of these symptoms, see your doctor for advice.
If you’re severely allergic to nuts or peanuts, your allergy may be triggered just by touching or being near someone who is eating them or has done recently. You may also have a reaction as a result of being in the same room where nuts have been. Using cutlery or crockery that has been contaminated with traces of nuts may also cause an allergic reaction.
Complications of food allergy
Some people develop a severe, whole-body allergic reaction called anaphylaxis, or anaphylactic shock; a rare but potentially fatal allergic reaction. Symptoms can include dizziness, a rapid pulse, a rapid drop in blood pressure and swelling of the airways and throat, making it difficult to breathe. If this happens you could lose consciousness if not treated.
Causes of food allergy
The exact reasons why some people are allergic to various foods aren't fully understood.
For some people with a food allergy, sensitivity may develop before birth while they are in their mother's womb (uterus). It's also possible that this may happen as a result of breastfeeding (although this isn’t the case for peanuts). Ask your doctor or your midwife or health visitor for information.
If you have other allergies or conditions such as eczema or asthma, you may be more likely to develop a food allergy. If someone else in your family has these conditions, this can also increase your risk of having an allergy, although it may not be to the same thing.
There is some evidence that some babies may become sensitised to nuts as a result of being treated with skin treatments for eczema or other allergic conditions that contain peanut oil, or from peanut oil found in certain sorts of formula milk and nipple creams.
Diagnosis of food allergy
Your doctor will ask about your symptoms and examine you. He or she may also ask you about your medical history.
If an allergy seems likely, your GP may refer you to a specialist allergy clinic for tests that may include the following.
• Skin prick tests – an extract of the suspect food is put on a small patch of skin, usually on your forearm or back, and a very small, fine scratch is made. If redness and swelling develops around the scratch, the test is positive for that food.
• Elimination and challenge diets – where you remove the suspected allergy food from your diet and replace it with another food. If your symptoms improve, a diagnosis can usually be made. To confirm this diagnosis, your doctor may ask you to re-introduce the food back into your diet. If you have had severe allergy symptoms in the past, this will be done under medical supervision in hospital.
• Blood tests – these are useful if you have a severe food allergy and are at risk of anaphylaxis from the tests above or if you have extensive eczema or dermatitis and can't have a skin test. The RAST (radioallergeosorbent) test measures levels of food-specific antibodies in your blood.
Treatment of food allergy
Some people outgrow their food allergies (especially children) but this is less likely with allergies to nuts and fish.
There isn't a cure for food allergy so the only way to prevent a reaction is to avoid the food you’re allergic to.
If you have a mild food allergy, it may be possible to treat this with antihistamines. However, it's important that you only take medicines for your allergy on the advice of your doctor. Always read the patient information leaflet that comes with your medicine and if you have any questions, ask your pharmacist for advice.
Emergency treatment
If you have a severe food allergy, you may be at risk of anaphylaxis and will need to take certain precautions. Despite reading menus and ingredients lists carefully, it's easy to eat a problem food by accident. Even a tiny amount of a problem food can trigger a severe reaction.
• Ask your doctor for advice about what to do if you have an allergic reaction.
• Let your family, friends and work colleagues know about your allergy, and how they can help you in the event of an emergency.
• Wear a bracelet or carry a card that gives details about your allergy.
• Carry a pre-loaded adrenaline syringe. Adrenaline is a hormone (a chemical that occurs naturally in your body) that relaxes muscles and so helps to reduce any swelling and make breathing easier. Single doses of adrenaline are available in the form of an EpiPen or AnaPen that consist of a sterile syringe of adrenaline that is ready to be used in an emergency. You will need to go to hospital immediately if you have anaphylaxis, even if using adrenaline has helped to reduce the reaction.
• If your child has a severe allergy, you must make sure that all their carers and teachers have the information to react correctly in an emergency.
Living with a food allergy
If you have a food allergy, it's important to check the packaging of foods carefully to find out if they contain what you’re allergic to. There are laws that food manufacturers have to work to that mean that all pre-packed food sold in the UK and the European Union must say on the label whether it contains an allergen, such as eggs or nuts. Attempts are being made to extend this to other foods that aren’t pre-packed.
If you’re allergic to eggs, you won't be able to have the vaccine for yellow fever. Your GP is also likely to advise you not to have the flu vaccine.
Published by Bupa's Health Information Team, August 2010.
Answers to questions about food allergy
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email.
How can I prevent my child from developing food allergies and will they grow out of them?
I have just been diagnosed with a peanut allergy – what precautions should I take with my meals?
I ate shellfish at a restaurant last night and have been sick and have a rash on my skin – is this a food allergy?
My daughter is allergic to eggs – is it safe for her to have the measles, mumps and rubella (MMR) vaccine?
Can I have the flu vaccine if I am allergic to eggs?
If I have a nut allergy, am I at risk of a reaction if I travel by plane?
Is it safe for me to eat or use products containing peanut oil if I have a peanut allergy?
I have a peanut allergy and I've heard I may be at risk of having an allergic reaction caused by lupins. Is this true?
How can I prevent my child from developing food allergies and will they grow out of them?
There are no proven ways to predict whether your child will have food allergies or to prevent your baby from developing them. However, a child born into a family with a history of allergies is more likely to develop food allergies than a child with no family history.
Explanation
Food allergies are more common in children than in adults. In most people, a food allergy won't continue into adulthood but will go or will be replaced by a different kind of allergy (such as an allergy to pollen, dust mites etc). The most common food allergies in children are to peanuts and tree nuts (such as Brazil nuts, hazelnuts and walnuts), cows' milk, eggs, wheat, fish and soya.
Pregnancy and breastfeeding
If you're pregnant or breastfeeding and are on a restricted diet because of a severe food allergy, you should check with your dietitian that you're getting all of the nutrients you need to stay healthy while pregnant or breastfeeding.
Babies are, to a certain extent, exposed to the foods eaten by their mothers when in the womb and during breastfeeding. The UK Government previously advised women not to eat peanuts during pregnancy and breastfeeding if there was a history of allergy in their immediate family. However, this advice was changed after research showed there was no clear evidence to say that eating or not eating peanuts during pregnancy affects the chances of your baby developing a peanut allergy. The UK Government is currently funding more research on peanut and other food allergies in the hope of improving our understanding of how allergies develop.
It has been shown that breast-fed babies are less likely to develop allergies or eczema than bottle-fed (with formula milk) babies. In the UK, it's recommended that babies are exclusively breastfed for the first six months of life. Breast-fed babies receive all the nutrients they need from their mother's milk, together with hormones and growth factors to help them develop, and antibodies which help protect them from infections.
Weaning
Talk to your health visitor about how and when to start introducing solid foods into your baby's diet (weaning). Usually, weaning isn't advised until a baby is six months old. When weaning your baby from breast or formula milk to solid foods, it’s important to introduce new foods gradually. It's best to introduce foods one at a time and watch your baby's response carefully – keeping a food diary may help to identify which foods your baby likes or dislikes, and any foods that cause any sort of reaction.
If you choose to start giving your baby solid foods before six months, don’t give them any type of nuts, seeds, milk, eggs, wheat, fish, shellfish, or foods containing these ingredients until after six months of age. This is because these foods can sometimes trigger development of a food allergy.
If your child already has an allergy, such as a diagnosed food allergy or eczema, or if there is a history of allergy in your child’s immediate family (if you or the father of your child or your other children have an allergy such as asthma, eczema or hayfever, your child has a higher risk of developing a peanut allergy. Talk to your GP or health visitor before you give peanuts or foods containing peanuts to your child for the first time.
Older children
Many children grow out of their food allergies by the time they are school-age. However, some allergies (including fish and peanut allergies) are more likely to continue into adulthood. If your child was diagnosed with a food allergy at an early age, it may be worth getting them re-tested in case their allergy has resolved.
Further information
• Allergy UK
01322 619 898
www.allergyuk.org
• Food Standards Agency
www.eatwell.gov.uk
Sources
• Peanut allergy. Food Standards Agency. www.eatwell.gov.uk, accessed 5 May 2010
• Adverse reactions to foods. British Nutrition Foundation. www.britishnutrition.org.uk, accessed 5 May 2010
• Peanut allergy. British Nutrition Foundation. www.britishnutrition.org.uk, accessed 5 May 2010
• Allergic reactions to food. Food Standards Agency. www.eatwell.gov.uk, accessed 5 May 2010
• Peanuts during pregnancy, breastfeeding and early childhood. Food Standards Agency. www.food.gov.uk, accessed 5 May 2010
• Improving the nutrition of pregnant and breastfeeding mothers and children in low-income households. National Institute for Health and Clinical Excellence (NICE), public health guidance 11, 2008
• Healthy child programme: pregnancy and the first five years of life. Department of Health. www.dh.gov.uk, accessed 5 May 2010
I have just been diagnosed with a peanut allergy – what precautions should I take with my meals?
After being diagnosed with any food allergy, it's important to get as much information as possible about how you can identify the problem food and what you should do if you're accidentally exposed to it.
Explanation
Ask your GP or allergy specialist to refer you to a dietitian who will show you how to identify problem foods and how to ensure you have a healthy, well-balanced diet without them.
UK and European Union (EU) law states that every pre-packed food must be clearly labelled to show whether they contain certain foods (or if one of its ingredients is made from, or contains one of these foods). Peanuts and tree nuts (including macadamia and Brazil nuts, pecans, cashews, pistachios, almonds, hazelnuts and walnuts) are among the foods which must be clearly labelled in this way.
Whenever you buy a pre-packed food, always check the label first, even if you have bought the product before – the recipe or method of manufacture might have changed since you last bought it. If you buy your groceries online, detailed product information and ingredient lists may not be available on the website – always check the labels of the products you have bought when they are delivered.
It's much more difficult to make sure that foods which aren't pre-packed don't contain peanuts or other problem foods. Examples of these are the foods that you might buy from sandwich shops, deli counters, salad bars, butchers, bakers or anywhere that food is weighed and sold loose. These foods won't have detailed ingredient and allergy labelling, and are also at increased risk of cross-contamination from foods that do contain peanuts or other problem foods. It may be safer, particularly if you have a severe allergy, never to buy foods which aren't pre-packed. Attempts are being made in the EU to extend current food labelling law to foods that aren’t pre-packed.
Eating out
If you're invited for a meal prepared by friends or family, make sure they are aware of your food allergy and which foods you can't eat. Ask them to check the ingredients they use with you. If appropriate, take your own food with you.
Before booking a table at a restaurant, it's important to inform the staff of your allergy and make sure that they can provide you with a meal that won't give you problems. When you arrive at the restaurant, tell the waiter, waitress and chef about your allergy and make sure they appreciate how serious it is. Don't rely on the menu for accurate descriptions of the dishes – nuts may be present in the food but not as a main ingredient and therefore may not be mentioned on the menu. Before ordering any food, carefully check the ingredients with the waiter or waitress and ask them to double check with the chef – preferably, you should speak to the chef yourself. If you’re in any doubt about a particular dish, don't order it.
Particular dishes to watch out for in restaurants are listed below.
• Malaysian, Chinese and Indian dishes – these often contain nuts or are cooked using nut oils.
• Salads – these can be garnished with nuts or dressed with nut oils.
• Desserts – nuts are often used as garnishes or may be present in the form of ground almonds or in the dessert base where they aren't immediately obvious.
• Food in self-service areas – these are at risk from cross-contamination (as in non pre-packed foods).
Before travelling and eating abroad, it's a good idea to learn how to tell people about your food allergy. Learn the words to look out for on menus and become familiar with local dishes that contain nuts. You can get translation cards in many different languages which will help you.
Medicines
It's important to check the ingredient lists of any medicines you take, whether this is off-the-shelf or over-the-counter from a pharmacy, or if it's a prescribed medicine. Your pharmacist can contact the manufacturer of your medicine to check whether the medicine contains peanuts (often as peanut oil), or if they are used in the manufacturing process.
Emergency treatment
If you have a severe allergy, you will probably have been prescribed an adrenaline pen (EpiPen or AnaPen) to use in case of accidental exposure to your problem food. Always carry the adrenaline pen with you and check it regularly to make sure it’s within the expiry date. It's very important that you're comfortable with using your adrenaline pen and are confident that you will be able to do so in an emergency. If you have any concerns about using your adrenaline pen, discuss them with your doctor and ask for more training on how to use it. If you ever have to use your adrenaline pen, it's vital that you seek urgent medical attention afterwards.
Make sure your friends, family and work colleagues are aware of your allergy and know what to do in an emergency.
If you need further information about your food allergy, talk to your GP or allergy specialist.
Further information
• Allergy UK
01322 619 898
www.allergyuk.org
• The Anaphylaxis Campaign
01252 542029
www.anaphylaxis.org.uk
Sources
• Understanding labelling rules. Food Standards Agency. www.food.gov.uk, accessed 6 May 2010
• Proposal for a regulation of the European Parliament and of the Council on the provision of food information to consumers. Commission of the European Communities, 2008, 2008/0028 (COD). www.ec.europa.eu
• Food allergy: how to avoid certain foods. Food Standards Agency. www.food.gov.uk, accessed 6 May 2010
• Food allergy and intolerance tips. Allergy UK. www.allergyuk.org, accessed 6 May 2010
• Allergic reactions to food. Food Standards Agency. www.eatwell.gov.uk, accessed 5 May 2010
• Self-administration of adrenaline (epinephrine). British National Formulary. www.bnf.org, accessed 5 May 2010
I ate shellfish at a restaurant last night and have been sick and have a rash on my skin – is this a food allergy?
Food allergy and food poisoning can often result in very similar symptoms and it can be difficult to know which of these conditions is causing your symptoms.
Explanation
Diarrhoea, feeling sick, vomiting and gastrointestinal discomfort can all be symptoms of both food allergy and food poisoning. However, there are some symptoms which you often get in food poisoning but not in food allergy and vice versa.
The common symptoms of food poisoning include diarrhoea, feeling sick, vomiting, abdominal (tummy) cramps, pain and fever.
The common symptoms of food allergy are diarrhoea, feeling sick, vomiting and bloating, but you may also, or instead, have coughing and wheezing, a runny nose, sore, red and itchy eyes, itching and/or swollen lips, mouth, tongue and throat and skin reactions (swelling, itching, rash, eczema).
These symptoms may also be caused by problems other than food allergy or food poisoning. Your GP is the best person to advise you as to whether you have a food allergy, food poisoning or another condition and what treatment you need.
In addition to thinking about the types of symptoms you're experiencing, consider the following points.
• If you have had similar symptoms with this type of food before, it's possible that you may have a food allergy or an intolerance to this type of food.
• If you have a history of allergic disease, or someone in your close family does, you're more likely to have allergies.
• If other people eating the same food have had similar symptoms, this suggests that there was a problem with the food itself. Contact the restaurant and/or your local environmental health department (through your local council office) to find out if they have had any other similar reports.
Further information
• Allergy UK
01322 619 898
www.allergyuk.org
• Food Standards Agency
www.eatwell.gov.uk
Sources
• Adverse reactions to foods. British Nutrition Foundation. www.britishnutrition.org.uk, accessed 5 May 2010
• Allergic reactions to food. Food Standards Agency. www.eatwell.gov.uk, accessed 5 May 2010
• Gastroenteritis. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 16 May 2010
• Peanut allergy. Food Standards Agency. www.eatwell.gov.uk, accessed 5 May 2010
My daughter is allergic to eggs – is it safe for her to have the measles, mumps and rubella (MMR) vaccine?
Yes, it's fine for your daughter to have the MMR vaccine, although it's possible that she may be given it in a hospital under medical supervision.
Explanation
The measles part of the MMR vaccine is produced by growing it on cells from eggs. Therefore, there was previously some concern that people who have an egg allergy might react to the vaccine. However, studies have shown that if you’re allergic to eggs, you’re no more likely to have an anaphylactic reaction to the vaccine than if you aren't.
If your daughter has had an anaphylactic reaction to eggs, she is still able to have the vaccine. However, it's possible that she will need to go into hospital to have the injection so that if she does have reaction, she can receive emergency treatment quickly.
Further information
• Allergy UK
01322 619 898
www.allergyuk.org
• NHS immunisation information
www.immunisation.nhs.uk
Sources
• Immunizations – childhood vaccination programme. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 6 May 2010
Can I have the flu vaccine if I am allergic to eggs?
The flu vaccine is produced by growing a strain of the virus inside hens' eggs. Therefore, although the flu vaccine doesn't actually contain any egg, it's still likely that you won't be able to have it.
Explanation
To produce the flu vaccine, a strain of the virus is placed inside a hen's egg and left to grow. It's then killed and purified. The vaccine doesn't actually contain egg but it may have been contaminated with egg products. It's likely that your GP will advise you not to have the flu vaccine, unless you’re particularly at risk of complications if you develop flu.
If you decide to have the vaccine, you will probably be given it in hospital so you can receive emergency treatment if you do have a severe reaction. It's possible that you may be tested for egg allergy before being given the vaccine.
Further information
• Allergy UK
01322 619 898
www.allergyuk.org
• NHS immunisation information
www.immunisation.nhs.uk
Sources
• Immunizations – seasonal influenza. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 6 May 2010
• 14.1 Active immunity. British National Formulary. www.bnf.org, accessed 6 May 2010
If I have a nut allergy, am I at risk of a reaction if I travel by plane?
People with food allergies travel by air every day without any problems. However, there may be a risk in terms of your exposure to nuts so it’s important to take certain precautions.
Explanation
There is no definite evidence about the risks of travelling by plane to people with a nut allergy. However, it's thought that you’re no more likely to have an allergic reaction on a plane than elsewhere, provided you take the same care as you usually would.
The most likely reason for you having an allergic reaction while on a plane would be as a result of eating something that contains nuts or which has been contaminated with nuts during preparation. Some airlines will provide you with a special meal if you request this in advance, but you will need to confirm this when you check in and when you get on the plane. The best way to make sure your food is completely free of nuts and nut traces is to take your own with you.
It's possible that surfaces on the plane will have been contaminated with allergens as a result of other people eating nuts. If you’re worried about this, take something to wipe your table and seat when you board the plane.
If you have a severe allergy that means you may have a reaction by breathing in the allergen, some airlines will try to arrange for nuts not to be served on the plane. Not all airlines will do this so always check with your airline before you book your flight. It's important to give as much notice as possible if you’re going to request this. You should remember that it's not possible to guarantee that other passengers won't bring nuts on board.
Always make sure you have your medicines with you and speak to your GP or allergy specialist before travelling by plane.
Further information
• Allergy UK
01322 619 898
www.allergyuk.org
Sources
• Staying safe while flying. The Food Allergy and Anaphylaxis Network. www.foodallergy.org, accessed 6 May 2010
Is it safe for me to eat or use products containing peanut oil if I have a peanut allergy?
This depends on whether the oil is refined or unrefined. If you have a peanut allergy, you’re unlikely to have an allergic reaction to refined peanut oil, and if you do it will probably be mild. However, you may be more likely to have a reaction to unrefined peanut oil.
Explanation
Research has shown that if you have a peanut allergy, you’re very unlikely to have a reaction to refined peanut oil. If the oil is refined, it means it has been treated to remove the part of the peanut which contains the allergen – the part that causes an allergic reaction. Unrefined peanut oil still contains this part of the peanut and is therefore more likely to cause an allergic reaction.
UK and European Union law states that food manufacturers must show on the label if a product contains peanut oil. However, they don't have to specify if this is refined or unrefined. There may also be products in the shops that were produced before this law was passed.
Refined peanut oil is found in many food products such as cakes and ready meals and in some skin care treatments such as those for eczema. Unrefined peanut oil isn't often found in food products, but it's possible that it may be used in some ethnic food products or in restaurant dishes to give them a peanut flavour. It's also important to look out for other names that may be used for peanut oil such as groundnut oil.
Further information
• Allergy UK
01322 619 898
www.allergyuk.org
• Food Standards Agency
www.eatwell.gov.uk
Sources
• Peanut allergy. Food Standards Agency. www.eatwell.gov.uk, accessed 5 May 2010
• Peanut allergy. The Food Allergy and Anaphylaxis Network. www.foodallergy.org, accessed 6 May 2010
• Understanding labelling rules. Food Standards Agency. www.food.gov.uk, accessed 6 May 2010
I have a peanut allergy and I've heard I may be at risk of having an allergic reaction caused by lupins. Is this true?
Yes, if you have a peanut allergy, it's possible that you may also react to lupins or products that contain lupin flour or seeds. This is because lupins contain many of the same allergens as peanuts.
Explanation
Lupins are legumes and are often found growing in gardens. They contain some of the same main allergens that can be found in peanuts. Therefore, if you’re allergic to peanuts, it's possible that you may also react to lupins.
Lupin seeds can be ground to produce flour or they may be used as an ingredient in foods such as seeded bread. Lupin flour is commonly used in mainland Europe as an ingredient in pastries and pasta and allergic reactions to it have been reported. If you’re allergic to peanuts, it's important to take care if you travel to Europe and be aware that certain food products may be more likely to contain lupin flour.
By law, all pre-packed food produced in the UK and the European Union must say on the label if it contains lupin.
Further information
• Allergy UK
01322 619 898
www.allergyuk.org
• Food Standards Agency
www.eatwell.gov.uk
Sources
• Peanut allergy. Food Standards Agency. www.eatwell.gov.uk, accessed 5 May 2010
• Lupin allergy. Food Standards Agency. www.eatwell.gov.uk, accessed 6 May 2010
Related topics
• Breastfeeding
• Coeliac disease
• Eczema
• Food hygiene
• Gastroenteritis
• Healthy eating
This information was published by Bupa’s Health Information Team and is based on reputable sources of medical evidence. It has been peer reviewed by Bupa doctors. The content is intended for general information only and does not replace the need for personal advice from a qualified health professional.
Publication date: August 2010.
Food allergy factsheet
Visit the food allergy health factsheet for more information.
Related topics
• Antihistamines
• Asthma
• Coeliac disease
• Eczema
• Healthy eating
Further information
• Allergy UK
01322 619 898
www.allergyuk.org
• Food Standards Agency
www.eatwell.gov.uk
• The Anaphylaxis Campaign
01252 542029
www.anaphylaxis.org.uk
Sources
• Allergic reactions to food. Food Standards Agency. www.eatwell.gov.uk, accessed 5 May 2010
• Food allergies. eMedicine. www.emedicine.medscape.com, accessed 5 May 2010
• Food allergy and intolerance. British Nutrition Foundation. www.britishnutrition.org.uk, accessed 5 May 2010
• Osborn DA, Sinn JKH. Soy formula for prevention of allergy and food intolerance in infants (Review). Cochrane Database of Systematic Reviews, 2006, Issue 4.
• Adverse reactions to foods. British Nutrition Foundation. www.britishnutrition.org.uk, accessed 5 May 2010
• Researchers successfully treat severe peanut allergy. Wellcome Trust. www.wellcome.ac.uk, accessed 5 May 2010
• Food allergy. DermNet NZ. www.dermnetnz.org, accessed 5 May 2010
• Peanut allergy. British Nutrition Foundation. www.britishnutrition.org.uk, accessed 5 May 2010
• Food allergy. National Institute of Allergy and Infectious Diseases. www.niaid.nih.gov, accessed 5 May 2010
• Peanut allergy. Food Standards Agency. www.eatwell.gov.uk, accessed 5 May 2010
• Peanuts during pregnancy, breastfeeding and early childhood. Food Standards Agency. www.food.gov.uk, accessed 5 May 2010
• Allergy and allergy tests: a guide for patients and relatives. The Royal College of Pathologists. www.rcpath.org, accessed 5 May 2010
• Skin prick testing. DermNet NZ. www.dermnetnz.org, accessed 5 May 2010
• Self-administration of adrenaline (epinephrine). British National Formulary. www.bnf.org, accessed 6 May 2010
• Understanding labelling rules. Food Standards Agency. www.food.gov.uk, accessed 6 May 2010
• Proposal for a regulation of the European Parliament and of the Council on the provision of food information to consumers. Commission of the European Communities, 2008, 2008/0028 (COD). www.ec.europa.eu
• 14.1 Active immunity. British National Formulary. www.bnf.org, accessed 6 May 2010
This information was published by Bupa’s Health Information Team and is based on reputable sources of medical evidence. It has been peer reviewed by Bupa doctors. The content is intended for general information only and does not replace the need for personal advice from a qualified health professional.
Publication date: August 2010.