Heart valve disease
This factsheet is for people who have heart valve disease, or who would like information about it.
Heart valve disease (also known as valve disease or valvular heart disease) means one or more valves in the heart aren’t working fully and blood isn’t flowing through the heart as it should.
About heart valve disease
Symptoms of heart valve disease
Complications of heart valve disease
Causes of heart valve disease
Diagnosis of heart valve disease
Treatment of heart valve disease
Special considerations
Living with heart valve disease
About heart valve disease
Heart valve disease can put extra strain on your heart and cause your heart to pump less efficiently.
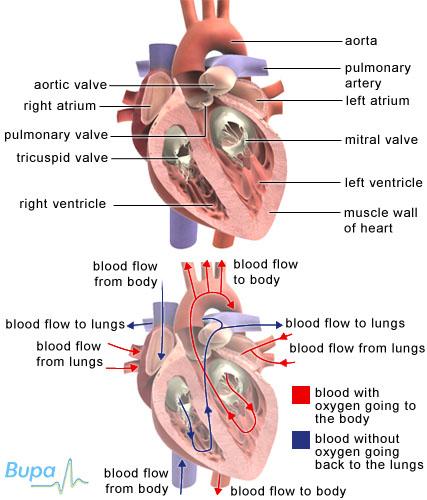
The heart
Your heart is a muscular pump that is divided into two sides. The right side of your heart pumps blood to your lungs to get oxygen, and the left side pumps the oxygenated blood around your body. There are two chambers on each side of your heart – the smaller atria and the larger ventricles.
Heart valves
There are four valves in your heart.
- Two are between the atria and the ventricles. The mitral valve on the left side and the tricuspid valve on the right.
- Two are in the arteries leaving the heart. The aortic valve on the left side and the pulmonary valve on the right.
Your heart valves are made up of flaps of thin strong tissue attached to the heart with fibrous cords. They can only open in one direction. Your heart valves have two functions.
- To help blood flow smoothly in one direction.
- To stop blood from leaking back against this flow.
Heart valve disease
Heart valve disease occurs when there is a problem with one of your valves.
- Valve stenosis – this is when your valve becomes narrow and your blood can’t easily flow into the next chamber or blood vessel. Your heart has to work harder to get blood through.
- Valve regurgitation (also known as valve insufficiency or incompetence) – this is when your valve doesn’t close properly and becomes leaky causing blood to flow in the wrong direction.
Symptoms of heart valve disease
The symptoms of heart valve disease depend on which valve is affected and how severely. If your valves are only mildly affected, you may not have any symptoms.
Symptoms of heart valve disease may include:
- breathlessness
- tiredness or fatigue
- palpitations (awareness of an irregular, fluttery heartbeat or a fast heart rate)
- angina (chest pain) because a diseased heart valve makes your heart work much harder
- swollen ankles or feet
- dizziness, fainting or blackouts
Complications of heart valve disease
If you have a damaged heart valve, it is more likely to become infected. Endocarditis is an infection of the heart lining. This can affect the heart valves and it can be very serious.
If you have heart valve disease, you may need to take antibiotics before you have surgery to reduce your risk of infection. Ask your GP for more advice.
Causes of heart valve disease
Heart valve disease can be caused by several conditions.
- Rheumatic fever during childhood. This causes inflammation of the heart muscles and although uncommon in the UK, it affects children in developing countries.
- Congenital heart valve defect. This means you were born with a faulty valve.
- Disease of the heart muscle (cardiomyopathy). You may have been born with this or developed it as a complication of another disease, such as rheumatic fever or endocarditis.
- Ageing. As you get older, your valves become less flexible, and more stretched or torn.
Diagnosis of heart valve disease
Your GP will ask about your symptoms and examine you. He or she may also ask you about your medical history. Your doctor may listen to your heart with a stethoscope to check for a murmur – an extra noise to the usual heart sounds. A murmur can be caused by blood passing through a damaged valve.
If your doctor suspects there may be a problem with your heart, you may have other tests in hospital.
- Echocardiogram (heart ultrasound scan) – to show the pumping action of your heart and the function of the heart valves.
- Chest X-ray – to rule out other conditions that may be causing your symptoms.
- Electrocardiogram (ECG) – to measure the electrical activity of your heart to see how well it’s working.
- CT scan or MRI scan – to provide detailed pictures of your heart muscles and valves.
- Angiogram (or cardiac catheterisation) – to see how well your heart valves and muscles are working and also to look at the coronary arteries.
Treatment of heart valve disease
Your treatment for heart valve disease will depend on what is wrong with your valve and how seriously it is affecting you.
Watchful waiting
If you only have mild heart valve disease, you may not need any treatment at all. You may still need regular check-ups to monitor your symptoms and ensure your heart valve isn’t deteriorating.
Medicines
You may be prescribed medicines to relieve your symptoms and slow down any worsening of the condition. The medicine you’re given will be the one that’s most effective for your individual needs.
- Diuretics (eg frusemide, spironolactone). These help to reduce swelling by encouraging your body to get rid of excess water in your urine. This should help you breathe more easily (by removing fluid in the lungs) and be more active (by reducing leg swelling).
- ACE inhibitors (eg ramipril, perindopril). These help your heart work more effectively by relaxing your blood vessels and so improving blood flow.
- Digoxin. This stabilises your heart rhythm and helps your heart pump harder.
- Warfarin. This is an anticlotting medicine that helps to reduce the risk of blood clots forming.
Surgery
Heart valve surgery
Your faulty heart valve may be replaced with an artificial valve (valve replacement) or your valve may be repaired if possible (valve repair). Both procedures are done under general anaesthesia. This means you will be asleep during the operation.
Balloon valve surgery (balloon valvuloplasty)
For children and younger people with a narrowed valve (stenosis), or adults who can’t have open valve surgery, your doctor may recommend balloon valve surgery.
A small tube (catheter) is threaded up to your heart through an artery, often from your groin. A guidewire, with a deflated balloon at the end, is passed up the catheter. When it reaches your narrowed valve, the balloon is gently inflated to stretch the valve. The balloon is then deflated and removed, leaving a widened valve that your blood can flow through more efficiently.
Special considerations
If you’re pregnant
During pregnancy, your heart needs to work harder. Your blood volume and heart rate increase and your resistance to blood flow decreases.
If you have heart valve disease and are keen to have a baby, your doctor may advise you to have valve surgery before you become pregnant.
Heart valve disease is sometimes first detected during pregnancy, because the extra strain on your heart means you get symptoms. If this happens, it’s usually possible to carry on with the pregnancy under careful medical supervision. Some medicines and types of surgery for heart valve disease are suitable even when you are pregnant.
Living with heart valve disease
If you have heart valve disease, you may have a yearly check-up with your cardiologist (a doctor specialising in identifying and treating conditions of the heart and blood vessels). This check-up is very important, even if you feel completely well. You might not need treatment for many years, if ever, but a careful, regular watch will make sure that you get any treatment you need at the right time.
Help and support
Contacting other people who have heart valve disease through charities and patient groups can be a good way to obtain support and advice.
What is mitral valve prolapse and do I need treatment?
I had a heart valve replaced and my doctor says I am at risk of endocarditis. What is this?
I have heart valve disease, are there any exercises that I shouldn’t do?
What is mitral valve prolapse and do I need treatment?
Mitral valve prolapse means there is a problem with the valve that separates the two chambers on the left side of your heart. About five in 100 people have a mitral valve that is slightly misshapen and leaks. If you have palpitations or chest pain, beta blockers may help.
Explanation
A mitral valve prolapse can be a cause of a heart murmur (a noise from your heart caused by turbulent blood flow) but it doesn’t usually cause serious problems. If you have a heart murmur, your GP will refer you to a cardiologist (a doctor specialising in identifying and treating conditions of the heart and blood vessels) to find out exactly what is causing it.
Mitral valve prolapses don’t usually have symptoms but you may have chest pain (angina) or palpitations (an unpleasant awareness of the heartbeat, often described as a thumping in the chest).
You won’t usually need treatment unless it’s causing you problems. Your GP may prescribe you beta blockers (eg bisoprolol fumarate) to help with your chest pain and palpitations.
If you have a mitral valve prolapse, there is a risk that your valve can become infected. If you’re going to have surgery or a test such as an angiogram, you may need to take antibiotics beforehand to reduce the risk of infection.
Further information
British Heart Foundation
0300 330 3311
www.bhf.org.uk
Sources
- Simon C, Everett H, van Dorp F. Oxford handbook of general practice. 2nd ed. Oxford: Oxford University Press, 2010: 267–68
- Prophylaxis against infective endocarditis. National Institute for Health and Clinical Excellence (NICE). March 2008. www.nice.org.uk
I had a heart valve replaced and my doctor says I am at risk of endocarditis. What is this?
Endocarditis is an infection in the lining of your heart. If you have a faulty or an artificial heart valve it can become infected and can result in heart failure if it isn’t treated quickly.
Explanation
Endocarditis is when the lining of your heart becomes inflamed usually because of a bacterial infection. Endocarditis is a serious condition that can cause heart failure if it isn’t treated quickly.
A faulty or an artificial heart valve is vulnerable to infection. When an infection occurs in the lining of your heart, it can spread to your heart valve and stop it from working properly.
Symptoms of endocarditis are sometimes similar to flu. You should seek medical advice as soon as possible if you have a heart condition and have any of these symptoms:
- fever
- sweats or chills
- aching muscles
- unintentional weight loss or loss of appetite
- breathlessness
- chest pain
Endocarditis can be treated with antibiotics. If your doctor suspects that you have endocarditis you will need hospital treatment.
If you have a heart condition, it’s important you take steps to reduce your risk of infection.
- Practice good dental hygiene and have regular dental checkups. This will help reduce the risk of bacteria entering your bloodstream through your mouth.
- Take care of your skin. Bacteria can enter your bloodstream through an infected break or cut in your skin. Wash any cuts or grazes carefully as soon as you notice them to prevent infection. Do not have any body piercing or tattooes.
For more information about preventing endocarditis, talk to your GP.
Further information
British Heart Foundation
0300 330 3311
www.bhf.org.uk
Sources
- Infective endocarditis. Map of Medicine. http://eng.mapofmedicine.com, published April 2010
- Simon C, Everett H, van Dorp F. Oxford handbook of general practice. 2nd ed. Oxford: Oxford University Press, 2010: 267–68
- Prophylaxis against infective endocarditis. National Institute for Health and Clinical Excellence (NICE). March 2008. www.nice.org.uk
I have heart valve disease, are there any exercises that I shouldn’t do?
Exercise is very good for your heart and overall health. It’s important to stay physically active if you have heart valve disease but you shouldn’t do any type of strenuous activity that brings on symptoms such as chest pain (angina) or palpitations.
Explanation
Your heart is a muscle and like the other muscles in your body it gets stronger with exercise.
If you have heart valve disease, talk to your GP about what type of exercise is best for you. You should increase your levels of physical activity gradually. You may be advised not to do any strenuous activities such as weightlifting and press-ups, or vigorous sports like squash, as these can put a strain on your heart. You should stop exercising immediately if you feel:
- shortness of breath
- pain
- dizzy or light-headed
- sick
If you develop any of these symptoms and they don’t go away after a few minutes you should see your GP.
Further information
British Heart Foundation
0300 330 3311
www.bhf.org.uk
Sources
- Physical activity and your heart. British Heart Foundation. www.bhf.org.uk, published August 2009
- Get active for your Heart. British Heart Foundation. www.bhf.org.uk, accessed 10 June 2010
Related topics
- Physical activity
- Caring for your teeth
Visit the heart valve disease health factsheet for more information.
Related topics
- Angina
- Arrhythmia (palpitations)
- Cardiovascular system
- Diagnosing heart conditions
- Heart attack
- Heart failure
- Heart valve repair surgery
- Heart valve replacement surgery
- Looking after your heart
Further information
British Heart Foundation
0300 330 3311
www.bhf.org.uk
Sources
- Vahanian A, Baumgartner H, Bax J, et al. Guidelines on the management of valvular heart disease. Eur Heart J 2007; 28:230–68
- Problems with valves. British Heart Foundation. www.bhf.org.uk, published May 2010
- Valvular heart disease. British Heart Foundation. www.bhf.org.uk, published May 2009.
- Physical activity and your heart. British Heart Foundation. www.bhf.org.uk, published August 2009
- Get active for your heart. British Heart Foundation. www.bhf.org.uk, accessed 10 June 2010
- Heart Failure – suspected. Map of Medicine. http://eng.mapofmedicine.com, published April 2010
- Valvular heart disease. Map of Medicine. http://eng.mapofmedicine.com, published July 2009
- Infective endocarditis. Map of Medicine. http://eng.mapofmedicine.com, published April 2010
- Simon C, Everett H, van Dorp F. Oxford handbook of general practice. 2nd ed. Oxford: Oxford University Press, 2010: 267–68
- Prophylaxis against infective endocarditis. National Institute for Health and Clinical Excellence (NICE). March 2008. www.nice.org.uk














