High blood pressure (hypertension)
This factsheet is for people who have high blood pressure (hypertension), or who would like information about it.
Blood pressure is a measure of the force that the blood applies to the walls of the arteries as it flows through them. It's normal for blood pressure to increase when you exert yourself, or when you feel stressed or anxious. But if your blood pressure is consistently higher than the healthy level when at rest, this is high blood pressure (hypertension).
Having your blood pressure taken
About high blood pressure
Symptoms of high blood pressure
Complications of high blood pressure
Causes of high blood pressure
Diagnosis of high blood pressure
Treatment of high blood pressure
Special considerations of high blood pressure
Having your blood pressure taken
About high blood pressure
Blood carrying oxygen and nutrients is pumped around your body by your heart. The blood is under pressure as a result of the pumping action of your heart and the size and flexibility of your arteries, which carry the blood. This blood pressure is an essential part of the way your body works.
You can get high blood pressure if the walls of your arteries lose their elasticity, become narrowed or contract too much, if your heart is pumping too much blood or if you have too much blood in circulation.
About three in 10 adults in the UK have high blood pressure. It's much more common in older people – seven out of 10 people over 75 have high blood pressure.
Symptoms of high blood pressure
Most people with high blood pressure don't have any symptoms.
If you have very high blood pressure, or your blood pressure rises quickly, you may have headaches, problems with your vision, fits or black-outs.
Complications of high blood pressure
If you have high blood pressure, you have an increased risk of major illnesses including:
• cardiovascular disease, such as angina (chest pain caused by reduced blood flow), stroke, heart attack, heart failure or atrial fibrillation (irregular heart beat)
• kidney damage
• damaged sight
Causes of high blood pressure
Primary hypertension
More than nine in 10 people with high blood pressure have what is called primary or essential hypertension. This means that it has no single clear cause.
Many factors to do with your lifestyle may contribute to primary hypertension. These include:
• smoking
• obesity (being very overweight)
• drinking a lot of alcohol – especially if you binge drink
• lack of exercise
• your diet
If someone else in your family has high blood pressure, you also have a higher risk of developing it.
Secondary hypertension
Around one in 20 people with high blood pressure have secondary hypertension. This means your doctor can link your high blood pressure to a known cause:
• kidney disease
• endocrine disease (hormone disorders – a hormone is a regulatory chemical that occurs naturally in your body)
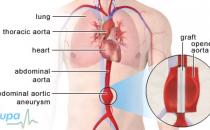
• a narrowing of the aorta (the largest artery leading from the heart) or the arteries leading to the kidneys
Secondary hypertension can also be caused by:
• steroid medicines
• the contraceptive pill
• pregnancy, which can cause pre-eclampsia – this can be serious and harm your baby
Diagnosis of high blood pressure
You may not have any symptoms, so your GP may diagnose high blood pressure when he or she takes your blood pressure as part of a medical examination. That's one good reason to have a regular check-up with your GP, especially if you're over 40.
Your GP or nurse will measure your blood pressure with a monitor called a sphygmomanometer. He or she will place a cuff around your upper arm and will inflate it to a certain level and then deflate it slowly.
The result is expressed as two numbers, such as 120/80mmHg (one hundred and twenty over eighty millimetres of mercury).
• The first figure – the systolic blood pressure – is a measure of the pressure when your heart muscle is contracted and pumping blood. This is the highest pressure in your blood vessels.
• The second figure – the diastolic blood pressure – is the pressure between heart beats when your heart is resting and filling with blood. This is the lowest pressure in your blood vessels.
The lower your blood pressure, the better for your health. Doctors recommend that your blood pressure is kept below 140/85. If you have diabetes or cardiovascular disease, your blood pressure should be lower than this – ideally less than 130/80. If your blood pressure is around this level, your GP will probably want to monitor it.
Your GP may ask you to come back for repeat measurements over a number of weeks before suggesting that you have treatment. This is so he or she can check that the high reading is an ongoing problem and not a one-off.
You may also need some tests to see if high blood pressure is affecting the rest of your body. These may include:
• a urine test – protein in your urine may be the first sign of a kidney problem
• a blood test to check your cholesterol and blood sugar levels, as well as the condition of your kidneys
• an electrocardiogram (ECG) – a test that measures the electrical activity of your heart to see how well it's working
Monitoring
You may be given a 24-hour monitoring if your GP thinks you may get ‘white coat’ hypertension – high blood pressure when a doctor or nurse measures it, or to find out what your blood pressure is overnight. A monitoring device is strapped round your waist and attached to a cuff wrapped around your upper arm. The cuff inflates and deflates automatically throughout the 24 hours and takes recordings of your blood pressure.
You might consider getting a blood pressure monitor to use yourself at home – discuss this with your GP. The British Hypertension Society (see Further information) can give you a list of clinically validated blood pressure monitors.
It's important to take readings on different days – for example you shouldn't just measure your blood pressure when you feel stressed. Set days in the week to take the measurement so that you can get a consistent reading.
You should continue to have your blood pressure tested regularly by your GP, even if you use a blood pressure monitor at home.
Treatment of high blood pressure
You're likely to need long-term treatment for high blood pressure because it can’t usually be cured.
If you have very high blood pressure, you may need to go to hospital for treatment. But it's much more likely that your GP and/or a nurse will look after you.
Self-help
Your GP or nurse will talk to you about lifestyle changes which might help. For example, he or she will advise you to:
• stop smoking
• change your diet to a low-fat, low-salt diet that includes fruit and vegetables
• cut down on alcohol
• cut down on coffee and high-caffeine drinks, such as cola
• take some regular, moderate exercise
• lose any excess weight
It may also help to try to reduce the stress in your life to prevent short-term rises in blood pressure – try relaxation techniques or meditation.
Medicines
If your blood pressure stays high, your GP may prescribe you one or more of the following antihypertensive medicines.
• ACE inhibitors (eg ramipril) or angiotensin-II receptor antagonists (eg candesartan cilexetil) – these relax and widen the walls of your blood vessels by reducing the production of hormones that cause your blood vessels to tighten.
• Calcium-channel blockers (eg amlodipine) – these help to widen your blood vessels by relaxing the muscles in your blood vessel walls.
• Diuretics (eg bendroflumethiazide) – these increase the amount of water and salt removed from your blood by your kidneys – lowering the volume of your blood which reduces blood pressure.
If your symptoms don’t improve after other medicines, then your GP may prescribe one of the following:
• Beta-blockers (eg atenolol) – these reduce the work your heart has to do by reducing your pulse rate and the force of contraction of your heart at rest and when you exercise.
• Alpha-blockers (eg doxazosin) – these help to widen your blood vessels by relaxing the muscles in the blood vessel walls.
The medicines your GP prescribes will depend on a number of factors, including your age and ethnicity. It may take time to find the best treatment for you; one that balances benefits against any side-effects.
It's important to take your medicines every day even if you don't have any symptoms of high blood pressure.
Special considerations of high blood pressure
Pregnancy
If you're pregnant your blood pressure is monitored regularly, whether you have hypertension or not. Long-term high blood pressure may be picked up at an antenatal appointment. It's also possible that you may develop high blood pressure during your pregnancy (gestational hypertension). High blood pressure that develops after 20 weeks of pregnancy can mean you have pre-eclampsia, which can be harmful for you and your baby.
If you have high blood pressure and think you may be, or are trying to become pregnant, it's important that you tell your GP. Certain medicines for treating high blood pressure aren't suitable for pregnant women.
Ethnic groups
If you're of African-Caribbean origin, you're at a higher risk of hypertension and you should visit your GP for regular monitoring.
You should also be monitored regularly if you're of South Asian origin because you have a higher risk of developing heart disease and diabetes.
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email.
Does stress cause high blood pressure and if so how can I reduce my stress levels?
Can I travel by plane if I have high blood pressure?
Can medicines cause high blood pressure?
Does stress cause high blood pressure and if so how can I reduce my stress levels?
Your blood pressure can rise if you're anxious or stressed. Long-term stress isn't thought to cause permanently high blood pressure. You may be able to help reduce your stress levels using relaxation techniques and exercise.
Explanation
Your blood pressure will change throughout the day and can increase if you become stressed or anxious. This can also happen if you get worried about seeing your GP to have your blood pressure measured – this is known as 'white coat’ hypertension. Your GP will want to take at least two measurements of your blood pressure to be certain that it's consistently high. Taking some measurements at home may help.
If your blood pressure rises when you're stressed, there are therapies you can try to help you control these short-term increases.
• You may find relaxation techniques such as meditation or yoga helpful.
• Stress management can help to prevent you getting stressed.
• Cognitive therapy (a type of talking therapy) can help you to focus on how you're feeling and how you cope with your problems.
Ask your GP for more advice about these therapies for blood pressure control.
By checking the results from a blood pressure monitor in different situations, you can see if your blood pressure is rising so that you can try to control it.
Further information
• British Hypertension Society
www.bhsoc.org
• British Heart Foundation
0845 070 80 70
www.bhf.org.uk
Sources
• Blood Pressure. British Heart Foundation. www.bhf.org.uk, accessed 22 September 2010
• Hypertension – not diabetic. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 23 September 2010
• Management of hypertension in adults in primary care. National Institute for Health and Clinical Excellence (NICE), 2006. www.nice.org.uk, accessed 23 September 2010
• Simon C, Everitt H, van Dorp F. Oxford handbook of general practice. 3rd ed. Oxford: Oxford University Press, 2010: 254
Can I travel by plane if I have high blood pressure?
Yes. Travelling by plane won't affect your blood pressure but you should consult your GP before you fly.
Explanation
Blood pressure isn't affected by air travel so it's perfectly safe for you to travel by plane if you have high blood pressure.
It's a good idea to consult your GP before you travel, especially if your blood pressure is unstable. Make sure that you have packed enough medicines to last you for your whole trip; you can get a prescription for up to three months from your GP. It's a good idea to pack some in your hand luggage and keep a note of your prescription or a letter from your GP in case your suitcase goes missing or if you get stopped at customs. You may have to pay a fee to obtain documents from your GP.
You should also be aware that travelling can be stressful, and this can cause your blood pressure to rise. Make sure you leave in plenty of time for your departure and don't pack too much as struggling with a heavy suitcase could also increase your blood pressure.
Further information
• Blood Pressure Association
www.bpassoc.org.uk
Sources
• Daily life with high blood pressure. Blood Pressure Association. www.bpassoc.org.uk, accessed 23 September 2010
Can medicines cause high blood pressure?
Yes. Certain medicines can cause high blood pressure.
Explanation
High blood pressure (hypertension) that has a known cause is called secondary hypertension.
Many substances and medicines can cause hypertension including:
• stimulants such as caffeine, nicotine and cocaine
• non-steroidal anti-inflammatory drugs such as etoricoxib
• the oral contraceptive pill and other hormone treatments
• some medicines used to treat anaemia, such as erythropoietin
• certain corticosteroids (fludrocortisone, cortisone, corticotropin and tetracosactide) used to treat a number of conditions
• certain medicines that are used to treat rheumatoid arthritis, for example ciclosporin and leflunomide
• certain herbal medicines that contain liquorice
• certain ingredients in some cough and cold remedies, such as ephedrine and phenylpropanolamine
• the antidepressant venlafaxine
Always consult your GP before you start taking any new medicines.
You should also be aware that certain medicines can interact with each other to cause hypertension. For example, some over-the-counter nasal decongestants contain ingredients that can interact with certain antidepressants to cause hypertension.
Always read the patient information that comes with your medicine and if you have any questions, ask your pharmacist for advice.
Sources
• Hypertension – not diabetic. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 23 September 2010
• Joint Formulary Committee, British National Formulary. 60th ed. London: British Medical Association and Royal Pharmaceutical Society of Great Britain, 2010. www.bnf.org, accessed 23 September 2010
Related topics
• Anaemia – a general overview
• Herbal medicine
• High blood pressure
• Hormonal contraception
• Menopause
• Rheumatoid arthritis
• Stress
• Stress in the workplace
Related topics
• ACE inhibitors and angiotensin-II receptor blockers
• Angina
• Beta-blockers
• Calcium-channel blockers
• Cardiovascular system
• Diagnosing heart conditions
• Diuretics
• Giving up smoking
• Healthy eating
• Healthy weight for adults
• Heart attack
• High cholesterol
• Looking after your heart
• Low blood pressure
• Pre-eclampsia
• Sensible drinking
• Stroke
• Type 1 diabetes
• Type 2 diabetes
Further information
• British Hypertension Society
www.bhsoc.org
• British Heart Foundation
0845 070 80 70
www.bhf.org.uk
Sources
• Hypertension – not diabetic. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 22 September 2010
• Hypertension. eMedicine. www.emedicine.medscape.com, accessed 22 September 2010
• Blood Pressure. British Heart Foundation. www.bhf.org.uk8, accessed 22 September 2010
• Simon C, Everitt H, van Dorp F. Oxford handbook of general practice. 3rd ed. Oxford: Oxford University Press, 2010: 252
• Hypertension in pregnancy. Clinical Knowledge Summaries. www.cks.nhs.uk, accessed 22 September 2010
• British Cardiac Society, British Hypertension Society, Diabetes UK, HEART UK, Primary Care Cardiovascular Society, The Stroke Association. Joint British Societies' guidelines on prevention of cardiovascular disease in clinical practice. Heart 2005;91:1–52 doi:10.1136/hrt.2005.079988
• Joint Formulary Committee, British National Formulary. 60th ed. London: British Medical Association and Royal Pharmaceutical Society of Great Britain, 2010. www.bnf.org, accessed 23 September 2010
• Management of hypertension in adults in primary care. National Institute for Health and Clinical Excellence (NICE), 2006. www.nice.org.uk, accessed 23 September 2010
• The management of hypertensive disorders during pregnancy. National Institute for Health and Clinical Excellence (NICE), 2010. www.nice.org.uk, accessed 23 September 2010