Endovascular aneurysm repair
This factsheet is for people who are planning to have endovascular repair for an aortic aneurysm, or who would like information about it.
Endovascular aneurysm repair (EVAR) is surgery to repair an aneurysm in the aorta (the largest blood vessel in your body) to stop it from bursting. An aneurysm is a widening or bulging of the aorta. EVAR is also known as stent grafting, as it involves inserting a graft mounted on slender metal tubes (stents).
You will meet the surgeon carrying out your procedure to discuss your care. It may differ from what is described here, as it will be designed to meet your individual needs.
About aortic aneurysms
Diagnosis of aortic aneurysms
What are the alternatives to EVAR?
Preparing for your operation
About EVAR
What to expect afterwards
Recovering from EVAR
What are the risks?
About aortic aneurysms
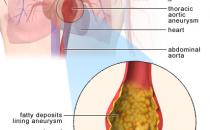
The aorta is usually 2 to 3cm (about one inch) in diameter. A weak spot in the aorta can cause it to bulge outwards (this is called an aneurysm). If the bulge occurs in the aorta as it goes through your chest, it’s called a thoracic aortic aneurysm. If it occurs in the aorta as it goes through your abdomen, it’s called an abdominal aortic aneurysm (AAA). AAAs are more common than thoracic aneurysms.
The chance of an aneurysm rupturing depends on its size. If your aneurysm is greater than 5.5cm wide, the chances of rupture are high – and the risk increases with increasing size. If an aneurysm bursts (ruptures), it can be fatal.
Diagnosis of aortic aneurysms
Aortic aneurysms often don’t have any symptoms, unless they are large or are growing quickly. Your GP may only suspect you have an aortic aneurysm following a routine examination.
If you’re a man over 65, you may be invited to be screened for an abdominal aortic aneurysm at your GP surgery or local hospital. The screening programme only covers abdominal aortic aneurysms, not thoracic aortic aneurysms.
Your surgeon will recommend surgery if your aneurysm is more than 5.5cm in diameter or causing symptoms.
What are the alternatives to EVAR?
Endovascular repair isn’t suitable for everyone. It depends on several factors, including the shape of your aneurysm, how near it is to other blood vessels and whether the arteries in your groin are large enough for the stent graft and the delivery device to be inserted.
Open surgery for aortic aneurysm (where your surgeon makes a cut in your chest or your abdomen) has been the standard procedure for many years. You may be advised to have this, rather than endovascular repair, which is a relatively new procedure.
Your surgeon will advise you which procedure is best for you.
Preparing for your operation
Your surgeon will explain how to prepare for your operation. For example, if you smoke you will be asked to stop, as smoking increases your risk of getting a chest and wound infection, which can slow your recovery.
The operation may be done under local anaesthesia. This completely blocks feeling in your groin (where the stent will be inserted) but you will stay awake during the operation. Alternatively, you can have a general anaesthetic and will be asleep during the operation. If you’re having a general anaesthetic, you will be asked to follow fasting instructions. This means not eating or drinking, typically for about six hours beforehand. However, it’s important to follow your anaesthetist’s advice.
Your surgeon will discuss with you what will happen before, during and after your procedure, and any pain you might have. This is your opportunity to understand what will happen, and you can help yourself by preparing questions to ask about the risks, benefits and any alternatives to the procedure. This will help you to be informed, so you can give your consent for the procedure to go ahead, which you may be asked to do by signing a consent form.
About EVAR
A stent – a metal tube that is covered with synthetic graft material – is fed through the femoral arteries in your groin up though the aorta to the area of the aneurysm. The stent comes pre-loaded on a delivery system, which will be used to position the stent graft correctly.
Your surgeon will make small cuts in your groin and will pass guide wires up the femoral arteries until they reach the aorta. Your surgeon will use X-ray images to guide the wires, confirm the position of your aneurysm and put the stent graft in place. The graft material bonds with the arterial wall and the blood flows through the stent instead of the weakened aneurysm.
You will usually have a CT angiogram to check your blood is flowing correctly through the stent.
The cut in your groin is closed with dissolvable stitches.
What to expect afterwards
After the operation, you may be taken to an intensive treatment unit (ITU) where you will be closely monitored or you will be returned to your ward.
You will be given painkillers to help with any discomfort as the anaesthetic wears off.
You can expect to stay in hospital for about three days.
The length of time your stitches will take to dissolve depends on what type you have. However, for this procedure they usually disappear within a couple of months.
When you’re ready to go home, you will need to arrange for someone to drive you home. You may be given a date for a follow-up appointment.
Recovering from EVAR
If you need pain relief, you can take over-the-counter painkillers such as paracetamol or ibuprofen. Always read the patient information that comes with your medicine and if you have any questions, ask your pharmacist for advice.
It can take up to two weeks to make a full recovery, but this varies between individuals, so it's important to follow your surgeon's advice.
What are the risks?
Endovascular aneurysm repair is commonly performed and generally safe. However, in order to make an informed decision and give your consent, you need to be aware of the possible side-effects and the risk of complications.
Side-effects
Side-effects are the unwanted but mostly temporary effects you may get after having the procedure.
After EVAR, your groin area (where the stent was inserted) may feel sore for a few days.
Complications
Complications are when problems occur during or after the operation. The possible complications of any operation include an unexpected reaction to the anaesthetic, excessive bleeding or developing a blood clot, usually in a vein in the leg (deep vein thrombosis, DVT).
Other complications of EVAR are uncommon but can include:
- wound infection – you may need treatment with antibiotics
- graft migration – the graft may move from its position
- wire fracture or fabric tear – the wires or fabric of the stent graft may break
- limb thrombosis – one of the limbs of the stent graft may kink or block and cause swelling
- endovascular leak (or endoleak) – blood may leak outside the stent graft and increase pressure in the aneurysm
- kidney damage – depending on the location of the aneurysm, your kidney function may be affected
- graft infection – this is very rare, but serious, and usually means that your graft will have to be removed
You will need to have regular check-ups for the rest of your life after having endovascular repair.
The exact risks are specific to you and differ for every person, so we haven't included statistics here. Ask your surgeon to explain how these risks apply to you.
Is surgery the only option if I have an aneurysm?
Can I opt to have endovascular repair instead of open surgery?
What follow-up will I need?
How long will my stent graft last?
Is surgery the only option if I have an aneurysm?
Surgery is usually only recommended if your aneurysm is at increased risk of bursting. If the risk of this happening is low, your surgeon will carefully monitor your condition and may suggest you make some lifestyle changes.
Explanation
Because the operation itself carries some risks, surgery is usually only recommended if your aneurysm is at risk of bursting. If your aneurysm is small (less than 5.5cm), then it’s very unlikely to burst.
Your surgeon will probably suggest you have regular ultrasound checks to see if the aneurysm grows over time. Surgeons call this ‘watchful waiting’ or surveillance.
Your doctor may also suggest some other measures to try and stop your aneurysm from getting bigger or from bursting. These might include stopping smoking and taking medicines to control your blood pressure and cholesterol. This prevents the build-up of fatty deposits in your arteries – the main cause of aneurysms.
Further information
The British Heart Foundation
0300 330 3311
www.bhf.org.uk
Sources
- Aneurysms. Merck Manuals Online Medical Library. www.merck.com/mmhe, published January 2008
- Aortic aneurysms. The Society of Thoracic Surgeons. www.sts.org, accessed 21 March 2010
- Thoracic aortic aneurysm. Medlineplus. www.nlm.nih.gov, published May 2010
- Aortic aneurysm and aortic dissection. British Heart Foundation. www.bhf.org.uk, published January 2010
Can I opt to have endovascular repair instead of open surgery?
Your surgeon will advise you on whether open surgery or having endovascular repair will be better for you. Endovascular repair isn’t suitable for everybody.
Explanation
For some people, having endovascular repair isn’t possible, due to the location or shape of their aneurysm or size of the arteries in their groin. Even for those people who are suitable for the procedure, open surgery is still often considered to be the better option – especially for those who are young and otherwise fit. This is because there is a need for life-long follow-up after endovascular repair and a risk of needing further treatment, which outweighs the small benefit of having this type of procedure for many people.
Further information
The British Heart Foundation
0300 330 3311
www.bhf.org.uk
Sources
- Endovascular stent-grafts for the treatment of abdominal aortic aneurysms. National Institute for Health and Clinical Excellence (NICE), 2009. Technology Appraisal Guidance 167. www.nice.org.uk
- Abraha I, Romagnoli C, Montedori A, et al. Thoracic stent graft versus surgery for thoracic aneurysm. Cochrane Database of Systematic Reviews 2009, Issue 1. doi: 10.1002/14651858.CD006796.pub2
- Endovascular stent–graft placement in thoracic aortic aneurysms and dissections. National Institute for Health and Clinical Excellence (NICE) 2005. Interventional Procedure Guidance 127. www.nice.org.uk
- AAA – endovascular aneurysm repair (EVAR). Circulation Foundation. www.circulationfoundation.org.uk, accessed 23 March 2010
- Greenhalgh RM, Powell JT. Endovascular repair of abdominal aortic aneurysm. New Engl J Med 2008; 358(5):464–74. http://content.nejm.org
What follow-up will I need?
You will need regular check-ups for the rest of your life following endovascular repair.
Explanation
It is possible for complications to develop after this type of procedure. For example, the stent may move position or it may break. Because of this, you need lifelong follow-up to check that your stent is still in place and is working properly.
You will usually need to have a follow-up CT angiogram about a month after you first have your procedure, and again after about six months. A CT angiogram creates a three-dimensional picture of the body, and uses a dye to show up the aorta. Alternatively, you may have an ultrasound scan to check the stent. You will continue to need yearly checks after this.
If a problem is identified during one of your check-up appointments, you will be advised if you need to have further tests or surgery.
Further information
The British Heart Foundation
0300 330 3311
www.bhf.org.uk
Sources
- Endovascular stent-grafts for the treatment of abdominal aortic aneurysms. National Institute for Health and Clinical Excellence (NICE), 2009. Technology Appraisal Guidance 167. www.nice.org.uk
- Abraha I, Romagnoli C, Montedori A, et al. Thoracic stent graft versus surgery for thoracic aneurysm. Cochrane Database of Systematic Reviews 2009, Issue 1. doi: 10.1002/14651858.CD006796.pub2
- Thoracic aortic aneurysm. Emedicine. http://emedicine.medscape.com, published November 2009
How long will my stent graft last?
As endovascular repair is a relatively new procedure, doctors don't have much information on the durability of stent grafts over the long-term.
Explanation
There is a chance that you may need further surgery to replace your stent graft if you have had complications after the initial procedure, such as blood leaking out of the stent graft (an endoleak). However, it isn’t known how likely this is to happen over the long term, as researchers currently only have data on how people have fared over a period of a few years. In addition, it will depend on the type of stent graft that your surgeon uses – this is because scientists are constantly trying to develop new devices to improve durability.
This is why your surgeon will want to monitor your progress.
Further information
The British Heart Foundation
0300 330 3311
www.bhf.org.uk
Sources
- Abraha I, Romagnoli C, Montedori A, et al. Thoracic stent graft versus surgery for thoracic aneurysm. Cochrane Database of Systematic Reviews 2009, Issue 1. doi: 10.1002/14651858.CD006796.pub2
- Greenhalgh RM, Powell JT. Endovascular repair of abdominal aortic aneurysm. New Engl J Med 2008; 358(5):464-74. http://content.nejm.org
- Hoffer EK, Forauer AR, Silas AM, et al. Endovascular stent-graft or open surgical repair for blunt thoracic aortic trauma: Systematic review. J Vasc Interv Radiol 2008; 19(8):1153–64
Related topics
- Giving up smoking
- Healthy eating
- High blood pressure
- High cholesterol
- Open surgery for aortic aneurysm
Visit the endovascular aneurysm repair (EVAR) health factsheet for more information
Related topics
- Abdominal aortic aneurysm
- Angiogram
- General anaesthesia
- Local anaesthesia and sedation
- Open surgery for aortic aneurysm
- Thoracic aortic aneurysm
Further information
British Heart Foundation
0300 330 3311
www.bhf.org.uk
The Circulation Foundation
020 7304 4779
www.circulationfoundation.org.uk
Sources
- Endovascular stent-grafts for the treatment of abdominal aortic aneurysms. National Institute for Health and Clinical Excellence (NICE), 2009. Technology Appraisal Guidance 167. www.nice.org.uk
- Endovascular stent–graft placement in thoracic aortic aneurysms and dissections. National Institute for Health and Clinical Excellence (NICE), 2005. Interventional Procedure Guidance 127. www.nice.org.uk
- Abraha I, Romagnoli C, Montedori A, et al. Thoracic stent graft versus surgery for thoracic aneurysm. Cochrane Database of Systematic Reviews 2009, Issue 1. doi: 10.1002/14651858.CD006796.pub2
- NHS abdominal aortic aneurysm screening programme. UK Screening Portal. www.screening.nhs.uk, accessed 23 March 2010
- Aneurysms. Merck Manuals Online Medical Library. www.merck.com/mmhe, published January 2008
- Aortic aneurysms. The Society of Thoracic Surgeons. www.sts.org, accessed 21 March 2010
- Aortic aneurysm and aortic dissection. British Heart Foundation. www.bhf.org.uk, published January 2010
- AAA – endovascular aneurysm repair (EVAR). Circulation Foundation. www.circulationfoundation.org.uk, accessed 23 March 2010
- Aortic aneurysm repair – endovascular. Medlineplus. www.nlm.nih.gov, published May 2010