Atrial fibrillation
Atrial fibrillation is when the heart beats too fast in an irregular rhythm. It is caused by faulty electrical signals in your heart and is the most common type of arrhythmia (irregular heartbeat).
The different types of arrhythmia
About atrial fibrillation
What happens in atrial fibrillation?
Symptoms of atrial fibrillation
Complications of atrial fibrillation
Causes of atrial fibrillation
Diagnosis of atrial fibrillation
Treatment of atrial fibrillation
The different types of arrhythmia
The information on the video provided does not constitute advice on diagnosis or the treatment for heart disease and such advice should always be sought from a doctor or another suitably qualified health professional.
About atrial fibrillation
Your heart is a muscular pump, responsible for delivering blood to the rest of your body. When your heart doesn’t beat in a normal way, it can’t do this as efficiently.
Atrial fibrillation affects around 800,000 people a year in the UK. The condition mostly occurs in older people, affecting about seven in 100 people over the age of 65, although it can happen in younger people as well.
What happens in atrial fibrillation?
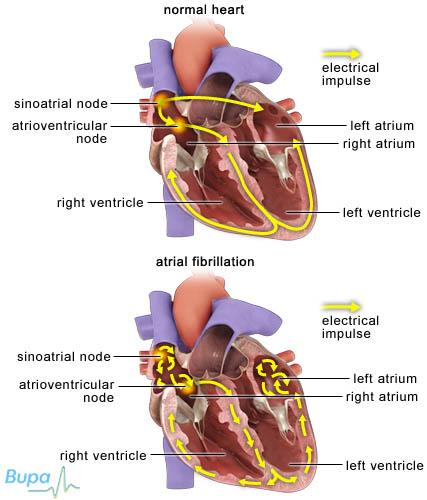
Your heartbeat is controlled by electrical signals (impulses), which travel through the heart making it contract. The signals travel from the atria (the upper chambers of the heart) to the ventricles (the lower chambers) through an area called the atrioventricular (AV) node. The AV node helps to synchronise the pumping action of the atria and ventricles.
Atrial fibrillation occurs when the electrical signals in the atria become disorganised, overriding the heart’s normal rate and rhythm. This causes the atria to contract irregularly or ‘fibrillate’.
There are three main types of atrial fibrillation:
• paroxysmal – it happens over seconds, minutes or up to 48 hours and the heart returns to a normal rhythm by itself or with treatment
• persistent – it requires electrical cardioversion to correct the rhythm
• permanent – even electrical cardioversion fails to restore the rhythm
Symptoms of atrial fibrillation
Symptoms of atrial fibrillation may include:
• palpitations – you’re aware of your heart beating faster or in an irregular way
• chest pain or discomfort
• shortness of breath
• dizziness and light-headedness
Many people with atrial fibrillation only have mild symptoms, or don’t have any symptoms at all.
These symptoms may be caused by problems other than atrial fibrillation. If you have them, visit your GP.
Complications of atrial fibrillation
Atrial fibrillation can cause a stroke and/or heart attack. This is because your blood isn’t flowing properly through your heart, so a blood clot can form. If a clot forms, it can block blood supply in your heart and cause a heart attack, or travel to your brain and cause a stroke. Because of this, people with atrial fibrillation are five times more likely to have a stroke than people without the condition.
If you have atrial fibrillation, you may need anticoagulant medicine (such as aspirin or warfarin) to prevent a clot forming.
Causes of atrial fibrillation
Many conditions that affect the heart or blood circulation can cause atrial fibrillation, including:
• high blood pressure
• heart valve disease
• heart muscle disease (cardiomyopathy)
• coronary heart disease
• congenital heart disease (problems of the heart since birth)
• inflammation of the heart (pericarditis)
• thyroid diseases
• lung cancer and chest infections
• a blood clot on the lung (pulmonary embolism)
Certain factors can also trigger temporary, reversible atrial fibrillation, including:
• alcohol
• being overweight
• caffeine
• certain medicines or drugs
• emotional or physical stress
• surgical procedures
Many people develop atrial fibrillation without having any underlying cause or risk factor. This is called lone atrial fibrillation.
Diagnosis of atrial fibrillation
Some people are not aware that they have fibrillation. If you have any concerns about your heart rhythm, see your GP. Your GP will ask about your symptoms and examine you. He or she may also ask you about your medical history.
Your GP will check your blood pressure, listen to your heartbeat and take your pulse. If your pulse is irregular, you are likely to have a test called an electrocardiogram (ECG). An ECG measures the electrical activity in your heart to see what the heart rhythm is.
If your GP suspects you have atrial fibrillation, he or she may refer you to a cardiologist – a doctor who specialises in identifying and treating heart and blood vessel conditions. You may have other tests in hospital, including:
• blood tests
• echocardiogram – an ultrasound scan of your heart providing a clear image of your heart muscles and valves that shows how well the heart is working
• ambulatory ECG – this takes a recording of your heartbeat while you go about your normal daily activities, usually over 24 hours
Treatment of atrial fibrillation
There are many treatment options available for atrial fibrillation. Your treatment will be tailored to you, and will depend on your own symptoms and the cause of your atrial fibrillation. Your doctor will discuss your treatment options with you.
The aim of treatment is to control your heart rhythm and rate, and reduce your risk of stroke or heart failure. You may not need any treatment at all, especially if your symptoms are mild.
Self help
Your doctor may suggest you improve your heart health by:
• exercising for 30 minutes every day
• eating a balanced diet with five portions of fruit and vegetables every day
• stopping smoking
• reducing alcohol and caffeine intake
Medicines
There are several different types of medicine that can help control atrial fibrillation, including beta-blockers, calcium channel blockers, anti-arrhythmic medicines and digoxin. They all work in different ways to control your heart rate or restore a normal rhythm.
Your doctor may prescribe a combination of any of these medicines. You may have to take them for just a short period until you have other treatment such as electrical cardioversion to restore your heart rhythm, or you may have to take them for months or years. Alternatively, you may be given medicine to take just when you get symptoms.
If your atrial fibrillation has come on suddenly, you may be given anti-arrhythmic medicine, as tablets or through a vein to try and get your heart rhythm back to normal (this is called chemical or medical cardioversion), and is usually given within 48 hours of having symptoms.
Medicines to reduce your risk of blood clotting are called anticoagulants. These include warfarin, heparin and aspirin. You will probably be offered one of these in addition to any other treatments you have.
Always ask your doctor for advice and read the patient information leaflet that comes with your medicine.
Electrical cardioversion
An electric shock is used restore your heart’s normal rhythm. It’s usually given if your symptoms have lasted longer than 48 hours and chemical cardioversion has failed. Electrical cardioversion is less likely to work if the arrhythmia has been present for over a year. It’s also not suitable if the irregular rhythm is coming and going, since it’s most likely that arrhythmia will return after treatment. For more information see related topics.
Surgery
Surgery is only used when your atrial fibrillation hasn’t responded very well to other treatments, and may include the following:
• Pacemaker – a small device is implanted under the skin near your collarbone. It monitors your heartbeat and produces electrical signals to prevent pauses in the heart rhythm.
• Catheter ablation – small tubes called electrode catheters are passed into your veins in the groin and threaded up to the heart. Abnormal tissue or the AV node, the junction box between upper and lower chambers (this is called AV node ablation) which is disrupting the electrical signals in your heart is burnt or frozen. You will also need a permanent pacemaker.
Answers to questions about atrial fibrillation
Will I get any side-effects from my medicine?
Are palpitations always caused by an arrhythmia?
Why might I need to have more than one catheter ablation?
Can I still exercise if I have atrial fibrillation?
Will I get any side-effects from my medicine?
All medicines have the potential to cause side-effects. Your doctor will discuss these with you before you start any treatment, so you can weigh up the risks and benefits of taking the medicine.
Explanation
• Although anticoagulants are very effective, they may thin your blood too much, causing you to bleed more than usual if you injure yourself. Other side-effects include: severe bruising, heavy bleeding during periods, bleeding gums and nose bleeds.
• The anti-arrhythmic medicine amiodarone can cause problems with your thyroid gland, lungs and liver; and make your skin very sensitive to sunlight. If you are prescribed amiodarone, you will have regular check-ups and will need to wear sunscreen and cover up in the sun more than usual.
• Beta-blockers can be associated with tiredness, coldness in your hands and feet, and disturbed sleep. More rarely, they can cause nausea, diarrhoea, rashes, impotence, nightmares and dizziness.
• Calcium-channel blockers can cause constipation, swollen ankles, low blood pressure and can trigger heart failure.
If you have any concerns about side-effects, talk to your doctor.
Are palpitations always caused by an arrhythmia?
No, there are many other causes of palpitations (where you become aware of your heart beating more rapidly or more forcefully).
Explanation
Most people experience palpitations at some time – including people without heart disease. While they can be unpleasant and distressing, these palpitations are normally harmless and go away on their own. Fear, anger, stress, physical activity, fever, stomach upsets, drinking alcohol or caffeine, tobacco and some medicines – including diet pills and cold medicines – may all cause palpitations.
You may also feel that your heart has skipped a beat or there’s an extra beat. An extra beat is called an ectopic beat and is very common. Extra beats are usually nothing to worry about and don’t need any treatment.
If your palpitations don't seem to have an obvious trigger, or are associated with other symptoms such as dizziness or chest pain, see your GP.
Why might I need to have more than one catheter ablation?
Sometimes, catheter ablation isn’t successful, and you may need to have a repeat procedure.
Explanation
Catheter ablation can treat atrial fibrillation in most people. However, some people may need more than one procedure for it to work. It’s also possible that the procedure may not completely cure your atrial fibrillation, but just reduce the number and duration of any symptoms you have.
The success of this procedure depends on:
• the type of atrial fibrillation you have
• the length of time you have had it
• whether or not you have any other heart disease
• the experience and the equipment available at the hospital where you have the procedure.
Can I still exercise if I have atrial fibrillation?
Exercise is generally encouraged, but you will need to discuss this with your doctor as it will depend on your individual circumstances.
Explanation
Generally speaking, exercise is good for the heart and is something that’s normally encouraged. However, atrial fibrillation may occasionally be triggered by exercise.
But research shows that doing light activities around the house and walking regularly – around three miles a week – helps older people with atrial fibrillation maintain a normal heart rate.
Once your doctor has got your atrial fibrillation under control with appropriate treatment, exercise will usually be safe. You may need to have an exercise electrocardiogram (ECG) first, to check how much you’re able to cope with. In this procedure, a recording of your heartbeat is taken while you exercise on a treadmill or exercise bike.
The following advice may help.
• Build up the amount of exercise you do at first very gradually. Always cool down.
• Exercise for 30 minutes at least five days a week or preferably every day. Half an hour can be broken into ten minute chunks.
• Do something you enjoy like gardening, walking or dancing or turn everyday tasks, like housework, into your daily exercise.
• Exercise until you feel warm and slightly out of breath.
• Always stop if you feel sick, dizzy or very breathless.
If you have heart disease, it’s sensible to speak to your doctor before starting any
Further information
-
Arrhythmia Alliance
01789 450787
www.heartrhythmcharity.org.uk
-
Atrial Fibrillation Association
01789 451837
www.atrialfibrillation.org.uk
-
The British Heart Foundation
0300 330 3311
www.bhf.org.uk
Sources
• Atrial fibrillation. Clinical Knowledge Summaries. www.cks.nhs.uk, published August 2009
• What is atrial fibrillation? Atrial Fibrillation Association. www.atrialfibrillation.org.uk, accessed 30 March 2010
• Atrial fibrillation. British Heart Foundation. www.bhf.org.uk, published June 2009
• Atrial fibrillation. Arrhythmia Alliance. www.heartrhythmcharity.org.uk, accessed 30 March 2010
• Heart rhythms booklet. Atrial fibrillation. British Heart Foundation.
www.bhf.org.uk, accessed 30 March 2010
• Atrial fibrillation. National Institute for Health and Clinical Excellence (NICE), June 2006. www.nice.org.uk
Related topics
• Arrhythmia
• Cardioversion
• Cardiovascular system
• Electrocardiogram (ECG)
Published by Bupa’s health information team, June 2010.















