Coronary angioplasty
Coronary angioplasty is a procedure used to unblock blood vessels that supply the heart with blood. Fatty material can build up on the inside of blood vessels. Coronary angioplasty flattens the fatty material against the wall of the blood vessel, which allows blood to flow more freely.
You will meet the doctor carrying out your procedure to discuss your care. It may differ from what is described here as it will be designed to meet your individual needs.
How coronary angioplasty is carried out
About coronary angioplasty
What are the alternatives?
Preparing for a coronary angioplasty
What happens during a coronary angioplasty
What to expect afterwards?
Recovering from a coronary angioplasty
What are the risks?
How coronary angioplasty is carried out
The information on the video provided does not constitute advice on diagnosis or the treatment for heart disease and such advice should always be sought from a doctor or another suitably qualified health professional.
About coronary angioplasty
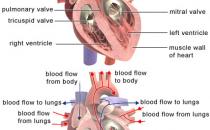
Your coronary arteries are blood vessels that supply your heart muscle with the blood and oxygen it needs to work properly. Over time a fatty substance, called atheroma, can build up inside your coronary arteries, causing them to narrow.
When your blood vessels become narrow, it means that less blood and oxygen reach your heart muscle. This can cause chest pain (angina [link to http://hcd2.bupa.co.uk/fact_sheets/html/angina.html]).
A coronary angioplasty is a procedure to open up any narrowed arteries so that blood can flow more easily to your heart. During the procedure, your doctor will gently inflate a small balloon in your artery and he or she may insert a stent to keep your artery open. A coronary angioplasty is sometimes called balloon angioplasty or percutaneous transluminal coronary angioplasty or intervention (PCTA or PCI).
You may have a coronary angioplasty to treat angina or after you have had a heart attack [link to http://hcd2.bupa.co.uk/fact_sheets/html/heart_attack.html]. You can have an angioplasty as a planned procedure or as an emergency procedure.
Some people may have an angioplasty straight after an angiogram. An angiogram is a test that allows your doctor to take an X-ray of your coronary arteries and find any narrowed areas.
What are the alternatives?
There are a number of alternatives to having coronary angioplasty.
If you have angina that has a regular pattern to it, for example, you have pain only when you exercise, it’s called stable angina. Stable angina can sometimes be controlled by medications and a change in lifestyle, for example, by being more active or stopping smoking.
If you have more severe and unpredictable angina or you have had a heart attack, then you may be offered an operation called coronary artery bypass grafting (CABG). CABG is an operation to bypass a narrowed section of your coronary artery using a blood vessel from your leg, arm or chest. You may need a CABG if you have too many narrowed sections of your coronary artery or if they are unsuitable for angioplasty.
Your doctor will refer you to a surgeon who will talk to you about the options available.
Preparing for a coronary angioplasty
Your doctor will explain how to prepare for your procedure. For example, if you smoke you will be asked to stop, as smoking increases your risk of the artery blocking again and slows your recovery.
If you’re having a planned coronary angioplasty, you may be able to have the procedure done and go home the same day. However, some people will need to stay overnight in hospital.
Angioplasty is usually done under local anaesthesia. You will have an injection of local anaesthetic where the needle will be inserted, either in your groin or arm. This completely blocks feeling in this area and you stay awake during the procedure. You may also be offered a sedative, which will help you to relax.
You will usually be asked not to eat or drink anything for about four hours before your angioplasty. You may be asked to stop taking some medicines, such as warfarin, a few days before the procedure. However, it’s important to continue taking your usual medicines unless your doctor tells you not to.
Your nurse may check your heart rate and blood pressure, and test your urine. You may be asked to shave your groin around the area where the needle will be inserted.
Your doctor will discuss with you what will happen before, during and after your procedure, and any pain you might have. This is your opportunity to understand what will happen, and you can help yourself by preparing questions to ask about the risks, benefits and any alternatives to the procedure. This will help you to be informed, so you can give your consent for the procedure to go ahead, which you may be asked to do by signing a consent form.
What happens during a coronary angioplasty
You will probably have your angioplasty in a specially equipped room called a catheterisation laboratory (or cath lab for short). The procedure lasts about 30 minutes, but may take longer depending on how many of your arteries need to be treated.
You will be given heparin during the procedure. This helps to stop your blood clotting.
Your doctor will make a small cut in your groin or wrist. He or she will thread a thin flexible tube, called a catheter, into the artery that leads to your heart. Once the catheter is in place a special dye (contrast medium) is injected. The dye is a colourless liquid but contains iodine which shows up on an X-ray. This shows the blocked areas of your blood vessels. You shouldn’t feel the catheter inside the blood vessels, but you may feel a warm sensation when the dye is injected.
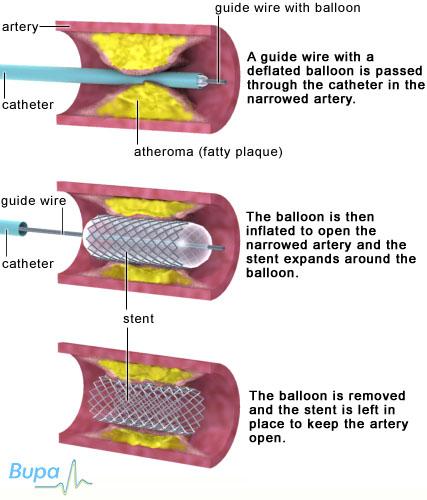
Your doctor will use X-ray images to guide a wire down the catheter. The wire is passed through the narrowed or blocked area and a small balloon (typically about 2cm by 3mm in diameter) is inserted along the guide wire and put into place across the narrowing or blockage. The balloon will then be gently inflated to squash the fatty material. This makes your artery wider and allows blood to flow more easily. The balloon will then be deflated and removed, along with the wire and the catheter. As the balloon is inflated in your artery, you may have some chest pain. This should get better quickly once the balloon has been deflated.
A stent is often used to keep your artery open after the balloon has been removed. A stent is a very small wire mesh tube. When the stent goes into your artery it’s in a collapsed form, but when the balloon inside is inflated the stent expands to fit against the artery walls. The balloon is then deflated and removed, leaving the stent in place in your artery.
Some stents are metal but others have a drug coating on them. The drug is then released slowly into your artery to stop it closing up again. Your doctor will decide whether to use a drug-coated stent depending on your condition and on the size and shape of the narrow artery. Your doctor may use a drug-coated stent if you have angina and if your artery is very narrow or the blockage is very long.
When the procedure is finished the catheter is removed from your artery. Your nurse or doctor will press firmly on the wound for about 20 minutes to make sure that the artery closes and any bleeding stops. A collagen plug (Angioseal) or similar device can be used to seal the hole in your artery. This means you may be able to get up sooner. In some cases, if you have had the procedure done through a cut in your groin, the tube that was used to introduce the catheter into your artery may be left in for a few hours. This allows any heparin given before the procedure to wear off, and prevents any bleeding. If you have had the procedure through your wrist, a tight band will be placed over the artery for a few hours.
What to expect afterwards?
After a coronary angioplasty you will need to rest for a while. Your nurse will check your blood pressure and pulse regularly. He or she will also check your wound to see whether it’s bleeding.
If you had the procedure done through a cut in your groin, you will need to stay in bed lying on your back for a few hours. If the procedure was done through a cut on your wrist, you will be able to sit up soon after the procedure.
You will need to arrange for someone to drive you home. You should try to have a friend or relative stay with you for the first 24 hours.
If you have had sedation, it will temporarily affect your co-ordination and reasoning skills so you must not drive, drink alcohol, operate machinery or sign legal documents for 24 hours afterwards. If you’re in any doubt about driving, contact your motor insurer, so that you’re aware of their recommendations, and always follow your doctor’s advice.
Your nurse will give you some advice before you go home. This includes information about:
• medicines, such as those that help to stop blood clots forming around the stent after your operation
• advice about how you can improve your diet and lifestyle once you get home
You may be given a date for a follow-up appointment.
Recovering from a coronary angioplasty
If you need pain relief, you can take over-the-counter painkillers such as paracetamol or ibuprofen. Always read the patient information that comes with your medicine and if you have any questions, ask your pharmacist for advice.
When you get home, you should check your wound regularly. You may have some bruising, but if swelling develops, or the area becomes hard to the touch or painful you should contact your doctor. If your wound starts to bleed, you should press firmly on it and contact the hospital straightaway.
It usually takes about a week to make a full recovery from a planned coronary angioplasty, but this varies between individuals, so it's important to follow your doctor's advice.
Depending on the type of work you do, you may be able to return to work after a few days.
You shouldn’t lift anything heavy for the first week after your angioplasty. You shouldn't drive for at least a week after angioplasty.
You may be asked to take medicines to help prevent your blood from clotting, for example aspirin or clopidogrel. You will usually need to take these for six months to a year after your angioplasty, depending on the type of stent you have had inserted.
If you had an emergency angioplasty, for example, after a heart attack, your recovery may take longer. Your doctor or nurse will be able to advise you.
What are the risks?
Angioplasty is commonly performed and generally safe. However, in order to make an informed decision and give your consent, you need to be aware of the possible side-effects and the risk of complications.
Side-effects
Side-effects are the unwanted, but mostly temporary effects you may get after having the procedure.
For the first few hours after your angioplasty, you may have some mild chest pain or discomfort. Tell your doctor or nurse if this happens.
You may have some pain or bruising where the catheter was inserted. If you have any redness, swelling or widespread bruising when you get home, contact your GP.
Complications of angioplasty
Complications are when problems occur during or after the procedure. Most people aren’t affected.
Specific complications of angioplasty are rare. These are listed below.
• Bleeding from the wound can sometimes be severe. If this happens you may need to have a small operation to repair the artery.
• Arteries treated with a stent can become narrow again. This is more likely to happen in the first few months after the procedure. If this happens, you may need to have another angioplasty.
• You might have an allergic reaction to the dye used during the procedure. This could be a rash, or it could be a more severe reaction which causes swelling and can affect your breathing. Your doctor will treat this quickly if it happens.
• Your coronary artery may become completely blocked during or soon after the procedure. You may need to have the angioplasty done again straightaway or you may, very rarely, need emergency heart surgery.
• The tip of the catheter can dislodge a clot of blood or fatty material from the wall of a blood vessel. These can block your artery, which may lead to a heart attack or stroke.
• The blood vessel being treated can be torn during the procedure. This may need an operation to repair it.
The exact risks are specific to you and will differ for every person, so we have not included statistics here. Ask your doctor to explain how these risks apply to you.
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email.
Is it safe for me to exercise after angioplasty?
How can I reduce my risk of further heart problems?
Will I still get chest pain (angina) after an angioplasty?
Is it safe for me to exercise after angioplasty?
Yes, but it's best to take things easy for the first few days after your coronary angioplasty. After that you can gradually increase the amount of activity you do. Your doctor will be able to tell you how much to do. Exercise can help to prevent further heart problems in the future.
Explanation
It’s safe for you to exercise after an angioplasty and it’s important for the long-term health of your heart for you to stay active.
You should spend the first few days after your angioplasty resting and doing gentle activity only, such as gentle walking or going up and down the stairs. This should be similar to the activity you were doing in hospital. After a few days, you can gradually build up the amount of activity you do and aim to do a little bit more each day.
Walking is a great way to do this and you can build up the distance you walk as the days go by. After a few weeks, you might want to try riding a bike or going for a gentle jog.
Don’t do strenuous activities such as weightlifting and press-ups, or very competitive sports such as squash.
If you become breathless or have chest pain when you’re exercising, you should stop and rest. If you have a GTN (glyceryl trinitrate) spray or tablets, make sure you take them with you when you exercise and use them if you have chest pain.
You may feel worried about being active after your angioplasty in case it makes your condition worse, or brings on a heart attack. These are natural worries to have. However, your heart is a muscle and it needs exercise to keep it fit. Your doctor or nurse will tell you how much exercise to do.
You may be invited to take part in a cardiac rehabilitation programme about four to eight weeks after having your coronary angioplasty. This will give you information about healthy eating, exercise and emotional support. A nurse, physiotherapist or exercise specialist will design an exercise programme for you, which will help to improve your fitness and health.
How can I reduce my risk of further heart problems?
If you have had coronary angioplasty, there are a number of things you can do to keep your heart healthy and improve the blood flow to your heart and the rest of your body. These include leading a healthy lifestyle and managing conditions such as high blood pressure.
Explanation
A coronary angioplasty isn’t a cure for heart disease. It opens up your arteries and improves the flow of blood to your heart muscle, but it can’t stop the build up of more fatty deposits in the future.
However, there are many things you can do that will help to keep your heart and your blood vessels healthy.
• If you're a smoker, then the best thing you can do for your heart is to stop. Talk to your nurse or GP about getting help to stop smoking.
• If you’re overweight, then losing excess weight can help to lower your risk of further heart problems. Eating a healthy diet and physical activity can help you to lose excess weight and maintain a healthy weight.
• Eating healthy foods will also help to prevent future heart problems. Eat at least five portions of fruit and vegetables a day. Eat foods that have low amounts of saturated fats in them and eat two portions of fish a week (one of them an oily fish, for example salmon or mackerel).
• Raised blood pressure and raised cholesterol levels can increase your risk of having a heart attack or stroke. Have your blood pressure and cholesterol levels checked regularly. If you have medicines for high blood pressure or raised cholesterol levels, make sure you take them as prescribed. Keep physically active. Choose something you enjoy and build activity into your day-to-day life.
Will I still get chest pain (angina) after an angioplasty?
Coronary angioplasty opens up the blood vessels that supply your heart muscle, but you may still get chest pain (angina) after an angioplasty. It’s important to know what to do if you develop angina and to always carry your GTN spay or tablets with you.
Explanation
For most people, angioplasty will improve the blood flow through the artery that has been treated. However, you may still get angina after the procedure.
If you have angina and you have a GTN (glyceryl trinitrate) spray or tablets, then you may be able to manage it yourself at home. The British Heart Foundation advises you to take the steps listed below if you develop angina.
1. Stop what you’re doing.
2. Sit down and rest.
3. Take your GTN spray or tablets following the instructions your doctor or nurse has given you. The pain should ease within a few minutes. If it doesn’t, take your GTN again.
4. If the pain doesn’t ease within a few minutes of taking the GTN a second time, call 999 immediately.
5. If you’re not allergic to aspirin, chew an adult aspirin tablet (300mg). If you don’t have an aspirin next to you, or you’re allergic to aspirin just stay resting until the ambulance arrives.
Chest pain can also be a sign of a heart attack. If you have any of the following, call for an ambulance straightaway.
• A crushing pain, tightness or heaviness in your chest.
• A pain in your arm, neck, back, jaw or stomach.
• You feel sick, sweaty, light-headed or short of breath.
Further information
• British Heart Foundation
0845 070 8070
www.bhf.org.uk
• The Circulation Foundation
020 7304 4779
www.circulationfoundation.org.uk
Sources
• Coronary Angioplasty. British Heart Foundation. Heart Information Series May 2009. www.bhf.org.uk
• Guidance on the use of coronary artery stents. National Institute for Health and Clinical Excellence (NICE), 2003, www.nice.org.uk
• Information for patients undergoing an angioplasty. The Royal College of Radiologists, March 2008. www.rcr.ac.uk
• Coronary artery stents. Understanding NICE guidance information for people with heart disease, their families and carers, and the public. National Institute for Health and Clinical Excellence (NICE), 2003, www.nice.org.uk
• Angioplasty and stent. Circulation Foundation. www.circulationfoundation.org.uk, accessed 17 August 2010
Related topics
• Angina
• Coronary angioplasty
• Cardiovascular system
• Coronary artery bypass graft (CABG)
• Coronary heart disease
• Diagnosing heart conditions
• Giving up smoking
• Healthy eating
• High blood pressure (hypertension)
• Heart attack
• High cholesterol
• Looking after your heart
• Physical activity
• X-ray