Ischaemic stroke
Published by Bupa's Health Information Team, February 2010.
This factsheet is for people who have had an ischaemic stroke, or who would like more information about it.
A stroke happens when the blood supply to the brain is interrupted. In an ischaemic stroke, the blood supply is blocked by a blood clot or clump of fat. It’s the most common type of stroke.
About ischaemic stroke
Symptoms of ischaemic stroke
Complications of ischaemic stroke
Causes of ischaemic stroke
Diagnosis of ischaemic stroke
Treatment of ischaemic stroke
Prevention of ischaemic stroke
About ischaemic stroke
In an ischaemic stroke, parts of your brain are starved of oxygen and nutrients when blood vessels become blocked. This damages brain cells and they begin to die. There are two different ways that an ischaemic stroke can happen.
• Arterial thrombosis. This is when a blood clot (thrombus) forms in a blood vessel supplying your brain and blocks the blood supply.
• Cerebral embolism. This is when a blood clot from somewhere else in your body (embolus) forms, travels to your brain and blocks the blood supply.
Your brain controls everything your body does, including your movements, speech, vision and emotions. Damage to your brain can affect any of these functions. After having an ischaemic stroke, about one in three people recover all or most of these functions.
Ischaemic strokes are most common in people over the age of 65, although they can happen at any age.
Symptoms of ischaemic stroke
Ischaemic stroke symptoms usually come on suddenly, within seconds or minutes. Less commonly, symptoms can come and go and get worse over several hours to a day or two.
A good way to recognise if someone has had a stroke is to use the face-arm-speech-time to call 999 test (abbreviated to FAST). This involves checking for any one of the three main symptoms of stroke – facial weakness, arm weakness or speech problems.
The exact symptoms of ischaemic stroke will depend on where in your brain the blood supply has been interrupted. For example, if a blood vessel that carries blood along the front of your neck to your brain becomes blocked you may have:
• blindness in one eye
• paralysis or weakness in one of your arms or legs, on one side of your body
• problems with understanding people or finding words when talking
Or, if a blood vessel that carries blood along the back of your neck to your brain becomes blocked, you may have:
• double vision
• weakness on both sides of your body
• dizziness and vertigo
If you notice that someone has any of these symptoms, you should call for emergency help straight away.
Complications of ischaemic stroke
Some ischaemic strokes may be mild and the effects only temporary, whereas others may be more severe and cause lasting damage. Complications of ischaemic stroke may include:
• weakness or paralysis, usually on one side of your body
• lack of awareness of one side of your body (usually the left side)
• loss of sensation on one side of your body
• difficulty swallowing
• extreme tiredness and sleep problems
• problems with speech, reading and writing
• problems with vision - such as double vision, or partial blindness
• memory and concentration difficulties
• difficulty controlling your bladder and bowel movements (incontinence) or constipation
• behavioural changes
Problems such as anxiety, depression and seizures (fits) can often improve as you recover.
If you’re unable to move because of stroke, you could be at risk of:
• bed sores (pressure ulcers)
• deep vein thrombosis (DVT)
• pneumonia
• contractures (altered position of your hands, feet, arms or legs because of muscle tightness)
Causes of ischaemic stroke
An ischaemic stroke happens when the flow of blood to your brain is interrupted either by a blood clot or clump of fat. The blockage may develop in one of the blood vessels in your brain (arterial thrombosis), or come from somewhere else in your body (cerebral embolus).
You’re at greater risk of getting a blood clot if your blood vessels have become narrowed and ‘furred up’ with fatty deposits – a process known as atherosclerosis. This often happens as people age. You can also develop atherosclerosis if you:
• smoke
• have uncontrolled high blood pressure
• have high cholesterol
• are overweight or obese
• have diabetes
• have a family history of stroke or heart disease
You're also at risk of ischaemic stroke if you have a type of abnormal heart beat (arrhythmia) called atrial fibrillation. In atrial fibrillation, your heart doesn't pump blood as efficiently and this can cause a blood clot to form in your heart.
The clot can then travel to your brain and cause a stroke. Regular, heavy drinking can put you at risk of developing an abnormal heart beat, as well as raise your blood pressure.
Diagnosis of ischaemic stroke
You will have a number of tests in hospital to try and find out what type of stroke you had and which part of your brain is affected. This will allow your doctor to plan your treatment.
[Please insert anchor links to the following underlined topic titles]:
You will have your blood pressure measured and an electrocardiogram (ECG) to record the rhythm and electrical activity of your heart. You may then have blood tests to measure your cholesterol and blood sugar levels, and to check for clots. You will also have a brain scan (eg a CT or MRI) as soon as possible.
Later on, you may have some other tests on your heart and blood vessels to find out what caused your stroke. These may include tests for blood clotting abnormalities and an echocardiogram (a procedure that uses ultrasound to produce a moving real-time image of the inside of the heart).
Treatment of ischaemic stroke
When you go to hospital, you may be treated on a general ward or in a specialist stroke unit.
If you're unable to swallow, you will be given fluid through a drip in your arm to stop you becoming dehydrated. You will have a tube in your nose to give you all the nutrients you need. You may also be given oxygen through a face mask, if you need it, to help you breathe.
You will be helped to sit up and move around as soon as you’re able. If you're unable to move, you will be helped to regularly turn in your bed, to reduce your chance of getting bed sores and DVT.
Medicines
You may be prescribed the following medicines for ischaemic stroke.
• Alteplase is a medicine used to break up blood clots and help restore the blood flow to your brain. It’s given through a drip in your arm within three hours of your symptoms starting. However, it may not be suitable for everyone.
• Aspirin, clopidogrel and dipyridamole are all medicines used to reduce your risk of blood clots forming after a stroke. You may be given one of these medicines as a tablet or via a feeding tube placed in your nose. Aspirin can also be given as a suppository - a medicine that is inserted into the rectum (back passage). These medicines may also be used for the long-term prevention of strokes.
• Warfarin and heparin are medicines which also prevent blood clots forming. They are mainly used to prevent strokes.
You may also be given some other medicines to control your blood pressure and to lower your cholesterol.
Surgery
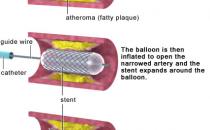
Your doctor may advise that you have surgery. This may involve having an operation to remove the fatty deposits from an artery in your neck (carotid endarterectomy). It may help to reduce your risk of having another stroke. You will usually have the operation within two weeks of your stroke. However, it’s only suitable for some people.
Rehabilitation
After a stroke, you may need to relearn skills and abilities, or learn new skills and adapt to the damage a stroke has caused. This is known as stroke rehabilitation.
Stroke recovery can be difficult to predict. Most people will make most of their recovery in the early weeks and months following the stroke. However, recovery can continue after this time.
The stroke team at the hospital will work out a rehabilitation programme for you that will be designed around your particular needs. This will continue after you leave hospital. Your rehabilitation programme may involve physiotherapists, speech and language therapists, occupational therapists, ophthalmologists and psychologists, as well as doctors and nurses.
Published by Bupa's Health Information Team, February 2010.
This section contains answers to common questions about this topic. Questions have been suggested by health professionals, website feedback and requests via email.
How long will my father have to stay in hospital after an ischaemic stroke?
If someone in my family had an ischaemic stroke, am I likely to have one?
Can taking aspirin prevent me from having an ischaemic stroke?
How long will my father have to stay in hospital after an ischaemic stroke?
It's difficult to predict how long someone will need to stay in hospital after any type of stroke. A team of health professionals can help you to decide on what care your father will need after he leaves hospital.
Explanation
The length of time someone needs to stay in hospital after a stroke varies from person to person and depends on the severity of their stroke. Someone who has had a stroke may need to stay in hospital for at least a week. If your father's stroke was severe, however, he may need to stay in hospital for a number of weeks, or even months.
Depending on your father's recovery in hospital, it may be that returning home isn't the best solution. Before he leaves the hospital, it’s likely that he will be seen by a team of health professionals. This may include a physiotherapist (a health professional who specialises in maintaining and improving movement and mobility), a speech and language therapist (a health professional who specialises in identifying and managing speech and communication problems) and a social worker. These people can help you think about the level of care your father needs and consider all available options. You may think about:
• sheltered housing - this is independent accommodation that has a resident warden on hand for emergencies
• a residential home - these provide basic personal care
• a nursing home - these have fully qualified nursing staff to provide 24-hour nursing care
There are a number of support groups and organisations you can contact if you need more advice about what care your father may need after leaving hospital. Speak to your social worker for further information.
If someone in my family had an ischaemic stroke, am I likely to have one?
You’re at greater risk of stroke if you have a family history of the disease. However, the chances of you having a stroke also depend on a number of lifestyle factors.
Explanation
You’re at greater risk of having a stroke if someone in your family has had one. However, this doesn't necessarily mean that you will have a stroke. Your risk of stroke depends both on factors that you can't change (such as your age, race and family history), and lifestyle factors, which you can change.
You can take the following steps to lower your risk of stroke.
• Stop smoking. Smoking increases your risk of developing atherosclerosis (narrowing and furring up of your arteries) and raises your blood pressure. Giving up can cut your risk of stroke in half, no matter how old you are or how long you have been smoking.
• Improve your diet. Too much fat in your diet can also contribute to the furring up of your arteries and too much salt can increase your blood pressure. A well-balanced, healthy diet can help to reduce your risk of stroke.
• Increase the amount of activity you do. If you’re overweight or obese, you’re more likely to have high blood pressure, heart disease or diabetes. Regular activity (30 minutes a day, five days a week) can help to lower your blood pressure and regulate the fat levels in your body.
• Reduce the amount of alcohol you drink. Regular, heavy drinking can raise your blood pressure and increase the likelihood of fatty deposits forming in your arteries. The Department of Health recommends that men drink no more than three or four units of alcohol a day and women no more than two or three units.
If you’re concerned or need further advice, speak to your GP to find out how you can change your lifestyle and reduce your risk of stroke.
Can taking aspirin prevent me from having an ischaemic stroke?
Research suggests that people who take aspirin as a preventive measure for stroke may not benefit in the long-term. To reduce your risk of stroke, you can change lifestyle factors such as your diet and activity levels.
Explanation
Aspirin is an antiplatelet medicine, which means it helps to prevent blood clots forming. However, it can also increase the chances of bleeding in your stomach and intestines. If you have never had a stroke before, the benefits of taking aspirin may not outweigh the risks of taking it long term.
You should only take aspirin to prevent a stroke if you have been advised to do so by your doctor. For example, if you have had an ischaemic stroke or a transient ischaemic attack (TIA) before, or if he or she thinks you're at risk, you may need to take regular doses of aspirin. Always read the patient information leaflet that comes with your medicine and if you have any questions, ask your pharmacist for advice.
Your GP may advise you to change some lifestyle factors, for example your diet and activity levels, to reduce your risk of stroke.
Further information
The Stroke Association
0303 303 3100
www.s
troke.org.uk
Sources
• Stroke information. The Stroke Association. www.stroke.org.uk, accessed 17 November 2010
• Ischemic stroke. The Merck Manuals. www.merck.com/mmhe, published November 2007
• Stroke, Ischemic. eMedicine. www.emedicine.medscape.com, published 4 June 2010
• Types of stroke. Chest Heart & Stroke Scotland. www.chss.org.uk, published 7 September 2010
• Personal communication, Dr Ahamad Hassan, Consultant Neurologist and Stroke Physician, Spire Leeds Hospital, 5 January 2011
• Stroke and TIA. Clinical Knowledge Summaries. www.cks.nhs.uk, published February 2009
• Stroke: Act F.A.S.T Awareness Campaign. Department of Health. www.dh.gov.uk, published 9 February 2009
• Stroke (CVA). The Merck Manuals. www.merck.com/mmhe, published January 2007
• Cardiovascular disease. British Heart Foundation. www.bhf.org.uk, accessed 14 December 2010
• Alcohol. British heart Foundation. www.bhf.org.uk, accessed 14 December 2010
• Simon C, Everitt H, van Dorp F. Oxford handbook of general practice. 3rd ed. Oxford: Oxford University Press, 2010:570–1
• Conditions NCCfC. Stroke: National clinical guideline for diagnosis and initial management of acute stroke and transient ischaemic attack (TIA). London: Royal College of Physicians, 2008:1-123
• Stroke rehabilitation. The Merck Manuals. www.merck.com/mmhe, published February 2009
• National clinical guideline for stroke. Royal College of Physicians. www.rcplondon.ac.uk, published 2008
• Joint Formulary Committee, British National Formulary. 60th ed. London: British Medical Association and Royal Pharmaceutical Society of Great Britain; 2010
• Alteplase for the treatment of acute ischaemic stroke. National Institute for Health and Clinical Excellence (NICE). www.guidance.nice.org.uk, published June 2007
• Stroke Unit Trialists' Collaboration. Organised inpatient (stroke unit) care for stroke. Cochrane Database of Systematic Reviews Issue 4. doi:10.1002/14651858.CD000197.pub2
• Factsheet 20: Accommodation after stroke. The Stroke Association. www.stroke.org.uk, published January 2007
• Antithrombotic Trialists’ (ATT) Collaboration. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. The Lancet, 2009; 373:1849–60
• Barnett H, Burrill P. Don’t use aspirin for primary prevention of cardiovascular disease. BMJ, 2010; 340(1805). doi:10.1136/bmj.c1805
• Lièvre M, Cucherat M. Aspirin in the secondary prevention of cardiovascular disease: an update of the APTC meta-analysis. Fundam Clin Pharmacol, 2010; 24(3):385–91. doi:10.1111/j.1472-8206.2009.00769.x
Related topics
• Cervical artery dissection
• Haemorrhagic stroke
• Ischaemic stroke
• Stroke
• Transient ischaemic attack (TIA)