Knee replacement
This factsheet is for people who are planning to have a knee replacement procedure, or who would like information about it.
Knee replacement involves replacing a knee joint that has been damaged or worn away, usually by arthritis or injury.
You will meet the surgeon carrying out your procedure to discuss your care. It may differ from what is described here as it will be designed to meet your individual needs.
How knee replacement is carried out
About knee replacement
What are the alternatives?
Preparing for a knee replacement
What happens during a knee replacement
Recovering from a knee replacement
What are the risks?
How a knee replacement is carried out
About knee replacement
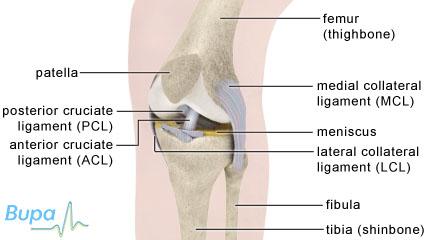
Your knee joint is made up by the ends of your thigh bone (femur) and shin bone (tibia). These normally glide over each other easily because they are covered by smooth cartilage. If your cartilage is damaged by injury or worn away by arthritis, for example, it can make your joint painful and stiff.
A new knee joint usually improves mobility and reduces pain, although your new knee will not be able to bend quite as far as a normal knee joint.
Depending on the condition of your knee joint, you may have part or all of your knee joint replaced. A total knee replacement is more common.
Artificial knee parts can be made of metal and/or plastic and a knee replacement can last for up to 20 years.
What are the alternatives?
Surgery is usually recommended only if non-surgical treatments, such as physiotherapy and exercise, taking medicines or using physical aids like a walking stick, no longer help to reduce pain or improve mobility.
Alternative surgical procedures include arthroscopy (if the arthritis isn’t too severe) or osteotomy (where the leg bones are cut and re-set). You may have already had these procedures before your knee replacement.
Your surgeon will explain your options to you.
Preparing for a knee replacement
Your surgeon will explain how to prepare for your operation. For example if you smoke you will be asked to stop, as smoking increases your risk of getting a chest and wound infection, which can slow your recovery.
The operation usually requires a hospital stay of about five days and it's done under general anaesthesia. This means you will be asleep during the operation. Alternatively you may prefer to have the surgery under spinal or epidural anaesthesia. This completely blocks feeling from your waist down and you will stay awake during the operation.
If you’re having a general anaesthetic, you will be asked to follow fasting instructions. This means not eating or drinking, typically for about six hours before a general anaesthetic. However, it’s important to follow your anaesthetist’s advice.
At the hospital, your nurse may check your heart rate and blood pressure, and test your urine.
Your surgeon will discuss with you what will happen before, during and after your procedure, and any pain you might have. This is your opportunity to understand what will happen, and you can help yourself by preparing questions to ask about the risks, benefits and any alternatives to the procedure. This will help you to be informed, so you can give your consent for the procedure to go ahead, which you may be asked to do by signing a consent form.
You may be asked to wear a compression stocking on the unaffected leg to help prevent blood clots forming in your veins (deep vein thrombosis, DVT). You may need to have an injection of an anticlotting medicine called heparin as well as, or instead of, stockings.
What happens during a knee replacement?
A knee replacement usually takes up to two hours.
Your surgeon will make a single cut (10 to 30cm long) down the front of your knee. He or she will move your kneecap to one side to reach the knee joint. Your surgeon will remove the worn or damaged surfaces from both the end of your thigh bone and the top of your shin bone. He or she will usually remove your anterior cruciate ligament and may remove your posterior cruciate ligament. For support, your surgeon won’t remove your collateral ligaments. He or she will shape the surfaces of your thigh and shin bones to fit the artificial knee joint and then fit the new joint over both bones.
Sometimes the back of your kneecap is replaced with a plastic part. This is called patellar resurfacing.
After your surgeon has fitted the new joint, he or she will close your wound with stitches or clips and cover with a dressing. Your surgeon will tightly bandage your knee to help minimise swelling.
You will need to rest until the effects of the anaesthetic have passed. You may not be able to feel or move your legs for several hours after an epidural anaesthetic.
You may need pain relief to help with any discomfort as the anaesthetic wears off.
For the first day or so, you may have an intermittent compression pump attached to special pads on your lower legs. By inflating the pads, the pump encourages healthy blood flow and helps to prevent DVT. You may also have a compression stocking on your unaffected leg. This helps to maintain circulation.
A physiotherapist (a specialist in movement and mobility) will usually guide you daily through exercises to help your recovery.
You will be in hospital until you can walk safely with the aid of sticks or crutches. When you’re ready to go home, you will need to arrange for someone to drive you.
Your nurse will give you some advice about caring for your knee and a date for a follow-up appointment before you go home.
The length of time your dissolvable stitches will take to disappear depends on what type you have. However, for this procedure they should usually disappear in about six weeks. Non-dissolvable stitches and clips are removed 10 to 14 days after surgery.
Recovering from a knee replacement
If you need them, you can take over-the-counter painkillers such as paracetamol or ibuprofen. Follow the instructions in the patient information leaflet that comes with the medicine and ask your pharmacist for advice.
The physiotherapy exercises are a crucial part of your recovery, so it's essential that you continue to do them for at least two months.
You will be able to move around your home and manage stairs. You will find some routine daily activities, such as shopping, difficult for a few weeks. You may need to use a walking stick or crutches for up to six weeks.
You may be asked to wear compression stockings for several weeks at home.
When you’re resting, raise your leg and support your knee to help prevent swelling in your leg and ankle.
Depending on the type of work you do, you can usually return to work after six to 12 weeks.
Follow your surgeon's advice about driving. You shouldn't drive until you are confident that you could perform an emergency stop without discomfort.
What are the risks?
Knee replacement surgery is commonly performed and generally safe. However, in order to make an informed decision and give your consent, you need to be aware of the possible side-effects and the risk of complications of this procedure.
Side-effects
These are the unwanted, but mostly temporary effects of a successful treatment, for example feeling sick as a result of the general anaesthetic.
Your knee will feel sore and may be swollen for up to six months.
You will have a scar over the front of the knee. You may not have any feeling in the skin around your scar. This can be permanent, but should improve over two years.
Complications
This is when problems occur during or after the operation. Most people are not affected. The possible complications of any operation include an unexpected reaction to the anaesthetic, excessive bleeding or developing a blood clot, usually in a vein in the leg (DVT).
Specific complications of knee replacement are uncommon, but can include those listed below.
- Infection of the wound or joint. Antibiotics are given during and after surgery to help prevent this.
- Unstable joint. Your knee joint may become loose and you may require further surgery to correct this.
- Damage to nerves or blood vessels. This is usually mild and temporary.
- Scar tissue. This can build up and restrict your movement. Further surgery may be needed to correct this.
The artificial knee joint usually lasts for 20 years, after which you may need to have it replaced.
The exact risks are specific to you and will differ for every person, so we have not included statistics here. Ask your surgeon to explain how these risks apply to you.
How long will my knee replacement last?
Are there any sports/activities I shouldn't take part in after my knee replacement?
What can I do to make my recovery easier?
How long will my knee replacement last?
Almost all knee replacements last at least 10 or 15 years, and some as long as 20 years.
Explanation
Replacements joints are designed to last for a long time. The modern materials used are strong enough to stand up to the requirements of young and active people.
Currently just over nine out of 10 artificial joints used for knee replacement last for 10 years or more. However, there is increasing research into the design and material of replacement knee joints to make them last longer.
You should have an X-ray on your knee at least every five years after your operation. If your replacement joint is loosening or breaking, you may need another operation to correct this.
Further information
-
British Association for Surgery of the Knee
www.baskonline.com -
The Arthritis Research Campaign (arc)
0300 790 0400
Sources
- Total knee replacement: a guide for patients. British Orthopaedic Association. www.boa.ac.uk, accessed 2 August 2010
- Knee surgery. Arthritis Research UK. www.arthritisresearchuk.org, accessed 2 August 2010
Are there any sports/activities I shouldn't take part in after my knee replacement?
Once you are fully recovered you can do exercise and sport. However you shouldn't take part in high-impact exercises such as running and jumping.
Explanation
During your recovery your physiotherapist will recommend exercises for you that will improve your strength and range of motion. You should do these for at least two months after your operation.
As you recover you can start swimming and do more walking to strengthen your muscles around the joint. You can gradually start cycling but if you feel any pain than you must stop and allow yourself more time to recover.
When you have made a full recovery, you can have a more active lifestyle. However it's important that you don't take part in high-impact activities or contact sports. So you shouldn't do sports such as football, rugby, basketball, squash, skiing or anything involving squats, jumping or weightlifting. But you can do low-impact sports such as golf, bowls or gentle doubles tennis or dancing.
Regular exercise will help to improve and maintain your mobility. When returning to any sport it's important to take your time to rebuild your strength and coordination.
You may find that you can't return to your chosen sport at the same level as you were before. Your risk of injury is greatly increased if you take part in competitive, rather than recreational, sport.
Your doctor, surgeon or physiotherapist will be able to give you more information about what activities are suitable.
Further information
-
The Arthritis Research Campaign (arc)
0300 790 0400
www.arthritisresearchuk.org
Sources
- Knee surgery. Arthritis Research UK. www.arthritisresearchuk.org, accessed 2 August 2010
- Activities after a knee replacement. American Academy of Orthopaedic Surgeons. www.orthoinfo.aaos.org, accessed 3 August 2010
- Total knee replacement: a guide for patients. British Orthopaedic Association. www.boa.ac.uk, accessed 2 August 2010
What can I do to make my recovery easier?
You should try to be as fit and healthy as possible before your operation and prepare your home for when you return.
Explanation
If you are having a knee replacement it's a good idea to try to be as fit and healthy as possible before your operation to speed up your recovery.
If you smoke you will be asked to stop, as smoking can increase your chances of getting a wound infection and slows your recovery. If you are overweight your doctor may recommend a weight-loss programme.
You can exercise to strengthen your upper body. This will help you to get around after the surgery when using walking aids such as crutches.
If it's possible you should try to strengthen your leg muscles. Strengthening the muscles around your knee will speed your recovery and will make it easier to perform the postoperative exercises.
Your surgeon or physiotherapist will be able to recommend exercises for you.
It's a good idea to prepare your home for when you return from hospital. This may mean rearranging furniture to make it easier to move around, and placing commonly used items at arm level so you don't have to reach for them. It's also a good idea to stock up on non-perishable food such as frozen or tinned items, so that you don't need to go shopping immediately after your surgery.
You may need someone to help during the first few weeks after surgery. It's a good idea to arrange to have a friend or family member stay with you for a couple of days after the operation.
Further information
-
The Arthritis Research Campaign (arc)
0300 790 0400
www.arthritisresearchuk.org
Sources
- Preparing for joint replacement surgery. American Academy of Orthopaedic Surgeons. www.orthoinfo.aaos.org, accessed 2 August 2010
Related topics
- Caring for surgical wounds
- Compression stockings
- Deep vein thrombosis
- Epidurals for surgery and pain relief
- General anaesthesia
- Knee arthroscopy
- Knee injuries
- Osteoarthritis
Further information
-
British Association for Surgery of the Knee
www.baskonline.com -
Arthritis Research Campaign (arc)
0300 790 0400
www.arthritisresearchuk.org
Sources
- Total knee arthroplasty. eMedicine. www.emedicine.medscape.com, accessed 22 August 2010
- Knee surgery. Arthritis Research UK. www.arthritisresearchuk.org, accessed 2 August 2010
- Total knee replacement. American Academy of Orthopaedic Surgeons. www.orthoinfo.aaos.org, accessed 29 July 2010
- Osteoarthritis. Clinical Knowledge Summaries www.cks.nhs.uk, accessed 29 July 2010
- Surgical treatment of osteoarthritis of the knee. American Academy of Orthopaedic Surgeons. www.orthoinfo.aaos.org, accessed 29 July 2010
- Is there any evidence that smoking impairs wound healing? Trip Answers. www.tripanswers.org, accessed 7 September 2009
- Total knee replacement: a guide for patients. British Orthopaedic Association www.boa.ac.uk, accessed 29 July 2010
- Jacobs W, Clement DJ, Wymenga AAB. Retention versus sacrifice of the posterior cruciate ligament in total knee replacement for treatment of osteoarthritis and rheumatoid arthritis. Cochrane Database of Systematic Reviews 2005. DOI: 10.1002/14651858.CD004803.pub2
- Activities after a knee replacement. American Academy of Orthopaedic Surgeons. www.orthoinfo.aaos.org, accessed 3 August 2010
















