Pancreatitis

This factsheet is for people with pancreatitis, or who would like information about it.
Pancreatitis is inflammation of the pancreas. There are two types of pancreatitis: acute – when the pancreas is inflamed and causes short-term illness; and chronic – when the pancreas is irreversibly damaged and causes ongoing long-term illness or bouts of acute symptoms.
About pancreatitis
Symptoms of pancreatitis
Complications of pancreatitis
Causes of pancreatitis
Diagnosis of pancreatitis
Treatment of pancreatitis
Prevention of pancreatitis
About pancreatitis
In the UK, up to 45,000 people are living with chronic pancreatitis and around 12,000 people get acute pancreatitis each year. Pancreatitis is more common in men than in women.
When describing an illness, the term ‘acute’ and ‘chronic’ refers to how long you have had it, not to how serious the condition is. An acute illness is typically over quite quickly. A chronic illness is one that lasts a long time, which may be for the rest of your life.
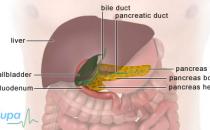
The pancreas
The pancreas is a 15cm (six inch) long organ that is part of your digestive system. It’s found just in front of your spine behind your stomach, at the level of your breastbone (sternum). It’s connected to the top of your small bowel (duodenum) by a tube called the pancreatic duct.
The pancreas produces digestive enzymes which help to break down food in your small bowel, and insulin – a hormone that helps to keep the level of sugar in your blood constant.
Symptoms of pancreatitis
Acute pancreatitis can be a life-threatening illness with severe complications. Symptoms come on suddenly or develop over a few days, and include:
- severe pain in the upper abdomen
- loss of appetite or feeling sick
- vomiting
- a temperature higher than 37.5°C
- yellowing of the skin and the white of your eyes (known as jaundice)
- a swollen abdomen (tummy)
If the inflammation is severe or recurrent your pancreas can have permanent damage, leading to chronic pancreatitis. Symptoms of chronic pancreatitis include the above, as well as:
- pale coloured, oily faeces
- unexplained weight loss and tiredness
These symptoms aren’t always caused by pancreatitis but if you have them, see your GP.
Complications of pancreatitis
Complications of acute pancreatitis can include:
- growth of fluid-filled cysts in the pancreas
- bleeding in the pancreas
- gallstones (small pebble-like stones made of hardened bile)
Complications of chronic pancreatitis can include the above, as well as:
- insulin-dependent diabetes
- slightly increased risk of having pancreatic cancer
Causes of pancreatitis
The most common causes of pancreatitis are:
- drinking excessive amounts of alcohol
- having gallstones in the bile duct
Other causes include:
- certain medicines, such as azathioprine and corticosteroids
- abdominal injuries
- a tumour in the pancreas
- an endoscopic ultrasound – see Diagnosis
- an infection with a virus, such as mumps or the Epstein-Barr virus
- increased calcium or lipid (fat) levels in your blood
- pancreas divisum – being born with ducts in the pancreas which don’t function properly
- genetics – you may inherit a faulty gene from your parents (this is called hereditary pancreatitis)
- cystic fibrosis
- inflammation of the blood vessels in your pancreas or reduced blood flow to your pancreas
Diagnosis of pancreatitis
Symptoms of acute pancreatitis can be severe enough to require immediate hospital treatment.
Your doctor will ask about your symptoms and examine you. He or she may also ask you about your medical history.
You may have blood tests to check levels of digestive enzymes – these can be at least three times the normal level. You may have the following scans to check the pancreas, gallbladder, and pancreatic and bile ducts.
- Abdominal ultrasound – sound waves and their echoes are used to to make pictures (or scans) of the inside of your body.
- CT scan – X-rays and computer software are used to create three-dimensional pictures of the inside of your body.
- Endoscopic ultrasound (EUS) – a camera attached to a flexible tube (endoscope) is passed down the throat, through your stomach, and into your small bowel. An ultrasound sensor produces soundwaves to create pictures of the pancreas and bile ducts. This procedure can sometimes trigger an attack of acute pancreatitis.
- Magnetic resonance cholangiopancreatography (MRCP) – this is an MRI scan, you will lie inside a cylinder-shaped scanner. A dye is injected into your vein that helps to show cross-section pictures of the pancreas and related organs.
Treatment of pancreatitis
Most people with acute pancreatitis need hospital treatment. Treatment usually consists of controlling pain, treating the inflammation and ‘resting’ the pancreas until symptoms improve. Depending on the severity of your symptoms and related complications you may need to stay in the intensive care unit (ICU) at the hospital.
If vomiting occurs, you will have a tube placed through the nose into your stomach to remove fluids and air.
When your symptoms have improved, your doctor will do further tests to determine the cause and degree of damage to your pancreas.
Chronic pancreatitis is managed by trying to prevent future attacks, making life-style changes to reduce the risk of further damage to your pancreas and by treating the damage that has already been done.
Medicines
You may need the following medicines to treat symptoms of acute pancreatitis:
- painkillers to relieve pain
- antibiotics to treat infection
You generally won’t be allowed to eat or drink until your symptoms improve. Pain medicines and antibiotics as well as fluids to keep you hydrated are usually given through a drip inserted into a vein in your hand or arm.
For chronic pancreatitis, your doctor may also prescribe medicines to help you manage your condition.
- Painkillers and/or antidepressants to relieve chronic pain.
- Synthetic pancreatic enzymes, such as pancreatin (eg Creon, Nutrizym, Pancrex) to replace the enzymes the pancreas can no longer make. You usually take these at meal times. Side-effects can include feeling sick, vomiting and discomfort in the abdomen.
- Insulin injections. If your pancreas isn’t producing enough insulin you may develop insulin-dependent diabetes. You will need daily injections of insulin to help control your blood sugar levels. For more information see Type 1 diabetes.
Always read the patient information leaflet that comes with your medicine and if you have any questions, ask your GP or pharmacist for advice.
Surgery
You may need surgery if your symptoms are caused by gallstones or if you develop complications, or if a large part of your pancreas is damaged. Surgery may be delayed until your symptoms have improved so that the risks associated with your operation are reduced.
Prevention of pancreatitis
You can help to prevent pancreatitis by eating a healthy diet and not drinking excessive amounts of alcohol.
Living with pancreatitis
If you have a bout of acute pancreatitis or are diagnosed with having chronic pancreatitis you will need to make lifestyle changes to help manage your condition and prevent further attacks.
Your doctor will suggest you drink sensibly and eat a low fat diet – a dietitian can help you plan an appropriate diet. You may also need to take vitamin supplements.
What life-style changes should I make after having pancreatitis?
Will chronic pancreatitis ever go away?
What is the risk of pancreatic cancer after chronic pancreatitis?
Does smoking cause pancreatitis?
How long will I stay in hospital with acute pancreatitis?
What should I do if it comes back?
What life-style changes should I make after having pancreatitis?
You should drink sensibly and eat a healthy low-fat diet.
Explanation
The most common causes of pancreatitis is drinking excessive amounts of alcohol. To help reduce your risk of having pancreatitis you should drink sensibly and eat a healthy low-fat diet.
If you’re diagnosed with chronic pancreatitis it’s even more important to start making changes to your eating and drinking habits. You may need to stop drinking alcohol altogether. Your doctor or dietitian can offer advice about your diet.
If your pancreas isn’t functioning properly, you may need to take pancreatic enzyme supplements to help digest food and you may need to take insulin to maintain your blood sugar levels.
Ask your GP for advice about managing your condition.
Sources
- Chronic pancreatitis. Merck Manuals Online Medical Library. www.merck.com/mmhe, accessed 17 March 2010
- Pancreatitis. National Digestive Diseases Information Clearing house (NDDIC). www.digestive.niddk.nih.gov, accessed 17 March 2010
Further information
The Pancreatitis Supporters’ Network
www.pancreatitis.org.uk
CORE charity
www.corecharity.org.uk
Will chronic pancreatitis ever go away?
No. Chronic pancreatitis can’t be cured.
Explanation
Once your pancreas is damaged its function is impaired forever. Chronic pancreatitis is a serious condition and it’s important that you get the treatment and guidance that you need.
Specialist doctors and nurses are experts in providing the care and support you need. There are support groups where you can meet people who may have similar experiences to you. Ask your doctor for advice.
Source
- Pancreatitis. National Digestive Diseases Information Clearing house (NDDIC). www.digestive.niddk.nih.gov, accessed 17 March 2010
Further information
The Pancreatitis Supporters’ Network
www.pancreatitis.org.uk
CORE charity
www.corecharity.org.uk
What is the risk of pancreatic cancer after chronic pancreatitis?
This depends on what has caused your chronic pancreatitis. About four in 10 people who have a rare inherited gene will develop pancreatic cancer.
Explanation
The risk of pancreatic cancer is higher if you have inherited a gene which causes chronic pancreatitis. This is called hereditary pancreatitis. If the cause of your chronic pancreatitis is alcohol, then the risk is much lower. Most people who develop pancreatic cancer don’t have pancreatitis.
Source
- Pancreatic cancer risks and causes. Cancer Research UK. www.cancerhelp.org.uk, accessed 19 March 2010
Further information
The Pancreatitis Supporters’ Network
www.pancreatitis.org.uk
CORE charity
www.corecharity.org.uk
Does smoking cause pancreatitis?
There is research that suggests smoking is linked to pancreatitis, but it’s not conclusive and more research is needed.
Explanation
Pancreatitis can be caused by a number of things and smoking may be linked to it. Smoking also increases the risk of pancreatic cancer. This is because smoke contains a chemical called nitrosamine which is thought to be linked to pancreatic cancer.
Sources
- Tolstrup JS, Kristiansen L, Becker U, et al. Smoking and risk of acute and chronic pancreatitis among women and men: A population-based cohort study. Arch Intern Med 2009; 169(6):603–9
- Yadav D, Hawes RH, Brand RE. Alcohol consumption, cigarette smoking, and the risk of recurrent acute and chronic pancreatitis. Arch Intern Med 2009; 169(11):1035–45
Further information
The Pancreatitis Supporters’ Network
www.pancreatitis.org.uk
CORE charity
www.corecharity.org.uk
How long will I stay in hospital with acute pancreatitis?
This depends on how severe your acute pancreatitis is and whether you develop any complications. Ask the doctor who is treating you for advice.
Explanation
You may need to be treated in the intensive care unit of the hospital after an attack of acute pancreatitis but you may then be moved to a different room or ward. Your doctor can advise you about how long he or she expects you to stay in hospital for your treatment.
Sources
- Pancreatitis. National Digestive Diseases Information Clearing house (NDDIC). www.digestive.niddk.nih.gov, accessed 17 March 2010
- Acute pancreatitis. Merck Manuals Online Medical Library. www.merck.com/mmhe, accessed 17 March 2010
Further information
The Pancreatitis Supporters’ Network
www.pancreatitis.org.uk
CORE charity
www.corecharity.org.uk
What should I do if it comes back?
If your symptoms come back you should visit your GP or go straight to the accident and emergency department at the hospital.
Explanation
Acute pancreatitis can be serious and will require hospital treatment. After you have had an attack of acute pancreatitis your doctor will do tests to try find out the cause. He or she may then be able to give you advice on how to prevent it re-occurring.
Sources
- Pancreatitis. National Digestive Diseases Information Clearing house (NDDIC). www.digestive.niddk.nih.gov, accessed 17 March 2010
- Acute pancreatitis. Merck Manuals Online Medical Library. www.merck.com/mmhe, accessed 17 March 2010
- Frossard Jl, Steer Ml, Pastor CM. Acute pancreatitis. The Lancet 2008; 371(9607):143–52
Further information
The Pancreatitis Supporters’ Network
www.pancreatitis.org.uk
CORE charity
www.corecharity.org.uk
Related topics
- Gallstones
- Giving up smoking
- Pancreatic cancer
Related topics
- Abdominal ultrasound
- CT scan
- Cystic fibrosis
- Gallstones
- MRI scan
- Mumps
- Pancreatic cancer
- Type 1 diabetes
Further information
The Pancreatitis Supporters' Network
www.pancreatitis.org.uk
CORE charity
www.corecharity.org.uk
Sources
- Pancreatitis. National Digestive Diseases Information Clearing house (NDDIC). www.digestive.niddk.nih.gov, accessed 17 March 2010
- Pancreatitis. Core. www.corecharity.org.uk, accessed 17 March 2010
- Pancreatitis. Lab Tests Online UK. www.labtestsonline.org.uk, accessed 17 March 2010
- Acute pancreatitis. Merck Manuals Online Medical Library. www.merck.com/mmhe, accessed 17 March 2010
- Pancreatitis. Emedicine. www.emedicine.medscape.com, accessed 17 March 2010
- Frossard Jl, Steer Ml, Pastor CM. Acute pancreatitis. The Lancet 2008; 371(9607):143–52
- Chronic pancreatitis. Merck Manuals Online Medical Library. www.merck.com/mmhe, accessed 17 March 2010
- Pancreatic cancer risks and causes. Cancer Research UK. www.cancerhelp.org.uk, accessed 19 March 2010
- UK working party on acute pancreatitis. UK guidelines for the management of acute pancreatitis. Gut 2005; 54:1–9
- Tolstrup JS, Kristiansen L, Becker U, et al. Smoking and risk of acute and chronic pancreatitis among women and men: A population-based cohort study. Arch Intern Med 2009; 169(6):603–9
- Yadav D, Hawes RH, Brand RE. Alcohol consumption, cigarette smoking, and the risk of recurrent acute and chronic pancreatitis. Arch Intern Med 2009; 169(11):1035–45